If you care for a loved one with dementia, you may have started to notice certain behaviors and symptoms that appear around sunset, such as agitation, pacing, wandering, and confusion. This is called sundown syndrome or sundowning. It can be extremely stressful both for the patient and their caregivers.
While there is no cure for sundowning, there are ways to manage symptoms with therapy, medication, and environmental adaptations to ensure the patient is comfortable and their physical needs are met.
Our treatment at Neural Effects can also help. Patients go through a combination of exercise and therapy sessions to promote cognitive skills and improve the patient’s quality of life. The sessions follow a consistent routine to help patients keep focus and engage in stimulating activities, which in turn reduces the risk of developing sundowning symptoms.
In this article, we’ll cover:
- What is sundown syndrome?
- What causes sundown syndrome?
- How is sundown syndrome diagnosed?
- How is sundown syndrome treated?
- What tips can help caregivers?
Neural Effects uses the latest evidence-based techniques to diagnose and help patients with dementia. We are located in Provo, Utah, and serve anyone in Salt Lake City or the Utah Valley area. We are an in-network provider with most types of medical insurance. Schedule your evaluation today.
What is Sundown Syndrome?

The term sundowning refers to a state of confusion that patients with dementia may experience at a specific time of day. It isn’t a disease by itself, but rather a group of symptoms that frequently manifest in the late afternoon and can last into the night. These symptoms affect at least 50% of dementia patients and can happen at any stage of dementia, but they are more common during the middle stage and later stages. It can affect patients with any type of dementia, including Alzheimer’s disease, Lewy body dementia, and other dementias, as well as patients with Parkinson’s disease.
Behaviors associated with sundowning include:
- Pacing
- Rocking in a chair
- Wandering
- Violence
- Shadowing (when patients follow their family caregiver around the house)
- Crying
- Yelling
- Agitation
- Anxiety
- Aggression
- Ignoring directions
- Confusion
- Paranoia
- Delusions and hallucinations
- Irritability
- Fear
- Mood swings
- Disorientation
- Abnormally demanding attitude
- Suspiciousness
- Visual and auditory hallucinations
These symptoms of sundowning can be very challenging for caregivers. Behavioral disruptions at the end of the day add to the stress at a time when caregivers may have to deal with other family commitments, such as meal times or homework with their children. Some sundown behaviors may also cause sleep disturbances, making patients more likely to wander and increasing the risk of sleep deprivation for caregivers. A tired caregiver is more likely to inadvertently use the wrong management strategies and aggravate sundown symptoms, triggering a vicious cycle for the entire family.
In addition, sundowning can lead to recurrent hospitalizations, prolonged hospital stays, and faster functional and cognitive decline.
As a result, sundown syndrome is one of the most common reasons families decide to move their loved one with dementia to a dementia care facility.
What Causes Sundown Syndrome?

The exact cause of sundown syndrome is yet unknown but is likely to be a combination of factors, including:
- Circadian rhythm disorders: According to multiple studies, sundowning is caused by disruption of normal circadian rhythm, which inevitably leads to behavioral issues. Changes in the hypothalamus caused by dementia alter the patient’s circadian rhythm and affect their body clock and sleep-wake cycle, which in turn triggers sundown symptoms. A second component involved in regulating the sleep-wake cycle is a hormone called melatonin. Levels of melatonin naturally decrease in geriatric patients, which may explain worsening sundown symptoms. This also explains the rationale for the use of melatonin in patients with dementia (more on this later).
- Sleep disorders: Problems sleeping are common in patients with dementia. These sleep problems include, for example, difficulty going to sleep or waking up frequently during the night. Although researchers don’t fully understand how sleep disturbances can cause sundown symptoms, there is some evidence connecting the two. The current theory is that changes in areas of the brain that regulate sleep affect the patient’s sleep-wake cycle and promote sundowning in patients with dementia.
- Environmental factors: Many environmental factors can cause sundown symptoms. For example, too much physical activity in the morning may cause fatigue in the afternoon and increase irritability and agitation. Another contributing factor is the lower staff-patient ratio for patients in care facilities or less available caregivers at home care in the evenings. Patients may notice less attention, which increases boredom and leads to agitation, restlessness, and other behavioral disruptions associated with sundowning.
- Medication: Sundowning symptoms may be a side effect of medication, such as hypnotics, antidepressants, and antipsychotics. These drugs may cause restlessness, agitation, and confusion, which cause or further aggravate sundowning symptoms. Many geriatricians and other healthcare professionals are against the use of benzodiazepines and other hypnotics to control nocturnal agitation, especially if the patient is on other medication. These drugs can cause drug dependence and increase the risk of respiratory problems.
- Other medical conditions: Patients suffering from other medical conditions are more likely to experience sundowning symptoms, especially if the patient is in pain and distress. It’s not uncommon for patients with depression or low mood to experience worse symptoms in the evening, which may explain some cases of sundowning. For some patients with diabetes, feeling hungry or having sudden changes in blood glucose levels (after a heavy meal, for example) may trigger agitation and confusion and lead to sundowning.
What Makes Sundowning Worse?
Independently of what causes sundown syndrome, some factors can make it worse, including if patients:
- Are tired, hungry, thirsty (or dehydrated), in pain, sleep deprived, or experiencing any other unmet physical needs
- Didn’t experience enough exposure to sunlight during the day
- Were overstimulated during the day, such as from a noisy or busy environment
- Are in an unfamiliar location
- Are sensory impaired, such as suffering from hearing or sight loss
- Are suffering from mood disorders, such as anxiety or depression
- Are experiencing the effects of fewer caregivers in a care home or limited availability of family members due to other commitments at home
- Are experiencing side effects of medication
- Are suffering from infections or other medical conditions
- Have poor or low lighting in their room and around the house
- Can see that their caregiver is stressed and frustrated, which may cause the person living with dementia to become stressed as well
- Are bored
How is Sundown Syndrome Diagnosed?

Diagnosis of sundown syndrome is entirely done based on symptoms described by the patient or their loved ones. The key is that symptoms appear (or get worse) during early evening or night. There are no blood tests or brain imaging scans that can confirm this diagnosis.
The only other condition that can be mistaken for sundown syndrome is called delirium. Symptoms of the two conditions are similar, but delirium only lasts a few days or months (typically while patients are fighting another medical condition, such as a urinary tract infection) and can affect patients at any time during the day. In contrast, sundowning is likely to affect patients for a long time, and symptoms only develop in the evening.
How is Sundown Syndrome Treated?

According to data from current medical research, the following pharmacological and non-pharmacological interventions can be effective in treating sundowning in patients with various forms of dementia:
Non-Pharmacological Options
Non-pharmacological approaches should be the first option considered to treat patients experiencing impairments caused by sundown symptoms. In general, these therapies are designed to reduce problematic behaviors, such as aggression and agitation, and counteract some of the factors that aggravate sundown symptoms, such as low stimulation during the day or poor exposure to sunlight.
- Light therapy: This therapy involves exposing the patient to a strong bright light to mimic sunlight. The idea is that increased exposure to light during the day (natural or artificial light) regulates the circadian rhythm and helps patients feel less agitated and confused. Studies show that light therapy can improve sleep, reduce the incidence of sundown episodes, and may even improve cognitive function. Patients may also feel better if they have a night light in their bedroom.
- Music therapy: In the later stages of dementia — when sundown symptoms are more likely to occur — patients with dementia may struggle to communicate with others, but they can still enjoy music. They may be able to hum along, try to follow the rhythm of the song with their hands, or simply listen to their favorite songs. Music therapy can reduce agitation and aggression, as well as improve mood and help patients engage more with their carers.
- Multisensory stimulation: In a sensory room, patients are exposed to objects that stimulate the five senses: different materials to touch, different smells, and different sounds, for example. The aim is to provide patients with a pleasurable sensory experience, and it can be used even if patients are in the later stages of the disease and struggling to communicate. This approach reduces the incidence of disruptive behavior and helps to keep patients calm. Some nursing homes offer multisensory rooms.
- Simulated presence therapy: This type of therapy is used mainly in care facilities. It involves playing personalized video or tape recordings of loved ones when older people are agitated or distressed. The content of the recordings varies according to the interests of the patient and includes shared memories or funny stories. Studies show that the recorded voice of a family member can be reassuring for the patient, reducing agitation and anxiety, as well as helping patients engage with their carers.
Environmental Interventions
In addition to non-pharmacological therapies, making sure the patient’s environment — including the bedroom and any other room in the house that the patient uses — is friendly and welcoming can reduce the incidence of sundown symptoms. Some suggestions include:
- Reducing noise: The main environmental recommendation to reduce the incidence of sundown symptoms in patients with dementia is to keep background noise low and minimize any unnecessary noise. This includes, for example, limiting noise from visitors, reducing banging in the kitchen, and keeping conversations in a low tone.
- Planning activities during the day: Other suggestions include having planned activities during the day to reduce disruptive behavior. Ideally, these activities should be planned at a time when patients are more likely to be agitated so they can work as a distraction. Keeping the patient active with a daily routine also promotes better sleep and provides opportunities to socialize and keep physically active.
- Meeting the patient’s physical needs: This includes making sure the patient is not scared, tired, hungry, thirsty, in pain, or anything else that may cause discomfort. Patients in the late stages of the disease may not be able to voice their needs, which results in them feeling confused and agitated. For example, caregivers should monitor what patients are watching on the television, especially in the evening. Anything frightening or violent can trigger disruptive behaviors, as patients may not be able to separate fact from fiction.
- Creating a relaxing environment: This is another useful way to reduce behavioral symptoms in patients with dementia. It can include, for example, listening to music or sounds of nature (waves, birds singing, etc), offering patients a snack or a drink in case they’re starting to get agitated because they’re hungry or thirsty, and generally talking to the patient with a soft and calming voice. Sometimes, just holding the patient’s hand is enough to lower anxiety.
Pharmacological Options
As a last resort, some patients may need medication to cope with their sundowning symptoms. This is particularly valid if the patients are at risk of harming themselves or others. Some options include:
- Melatonin: As we’ve described earlier, sundown symptoms can be caused by a disrupted circadian rhythm. One option to repair this disruption is by using melatonin. Several studies show that melatonin reduces sundowning behavior and nocturnal activity, decreases sleep latency, and improves quality of sleep.
- Acetylcholinesterase inhibitors: These prescription drugs are routinely used to treat patients, but there is no evidence to suggest they can help control sundowning symptoms. Some studies suggested that donepezil can aggravate nighttime behaviors and increase the risk of insomnia. Taking this drug in the morning may help counteract these effects.
- Antipsychotic medications: These drugs are a popular option for extreme cases of sundowning symptoms. They can reduce agitation and promote better sleep, as well as control more serious symptoms, including delusions, hallucinations, and paranoid ideas. While there are no studies specifically looking at antipsychotics for the treatment of sundowning symptoms, they’re considered effective for patients with dementia.
Treatment for Dementia at Neural Effects
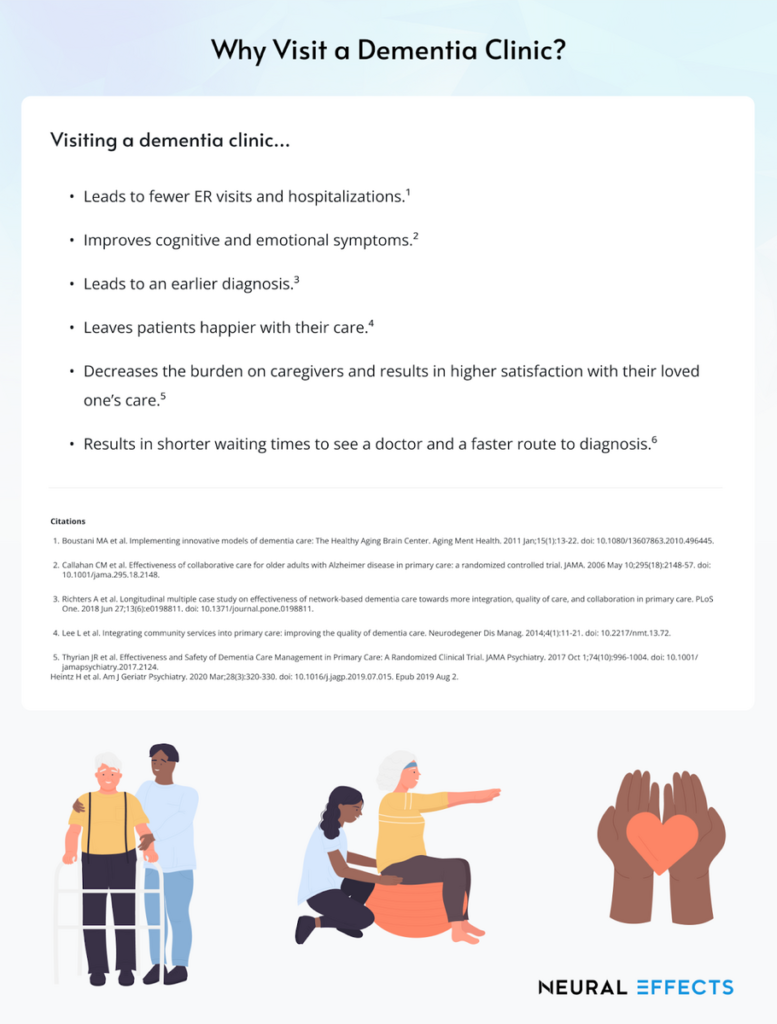
Another helpful option for caregivers and patients suffering from dementia is to get treatment at a dementia clinic — a medical facility where you can have symptoms related to memory loss and other cognitive skills investigated and treated by an expert.
During treatment at Neural Effects, we use a combination of physical exercise and cognitive stimulation therapy (CST) to delay cognitive decline and improve the patient’s quality of life. The aim is to allow patients to live independently for as long as possible.
Multiple studies prove that CST is one of the most effective ways to protect cognitive function and delay the progression of dementia symptoms. In addition to providing CST to our patients, we add short sessions of aerobic exercise to further increase the benefits of therapy. Exercise promotes the release of important chemicals in the brain, including one called brain-derived neurotrophic factor (BDNF), which stimulates learning and memory.
Treatment starts with a neuropsychological exam (also called a neurocognitive evaluation) to find out how dementia has affected the patient’s brain. Typically, this exam takes about 2–2.5 hours to complete. Our therapists assess:
- Cognitive skills, such as problem-solving ability, memory, attention, and concentration
- Physical abilities, such as reflexes, eye movements, and balance
- Emotional signs of anxiety, stress, and depression
After completing this exam, the information is combined and used to create a cognitive care plan (CCP). All patients we assess will receive their CCP, even if they decide not to continue with treatment. We feel this report contains valuable information to help patients protect their cognitive function and improve their quality of life.
The CCP includes:
- Results from the assessment
- Risk factors and how the disease is likely to progress
- Lifestyle changes that may help the patient
- Resources for the family and ways they can get involved
- Recommended treatment options
Patients can then start their group CST sessions. The treatment includes 14 one-hour sessions run twice a week for seven weeks.
Sessions start with a few minutes of aerobic exercise, usually done on a stationary bike or treadmill. Our therapists are trained to accommodate mobility issues and other health conditions that might affect how much exercise patients can do safely.
After exercise, patients may discuss current affairs, play board games, listen to music, or do arts and crafts. The theme for each session is different, but all sessions are run similarly to help patients keep their focus. Sessions also include orientation sections, where our therapists gently remind patients about date and time. Overall, CST helps with cognitive skills, such as memory, thinking, and language. It boosts confidence and improves quality of life.
At the end of the treatment, if our therapists feel that patients would benefit from additional therapy, we refer them as needed to the appropriate specialists.
Lastly, we recognize that being a caregiver can be extremely challenging, especially if patients exhibit disruptive behaviors such as sundowning syndrome. Family members and caretakers can attend the first session to learn more about CST. This helps them repeat some of the exercises and games at home with their loved ones. Our therapists also give family members additional information regarding local resources and lifestyle changes that can help their loved ones maintain independence for longer.
Tips for Caregivers to Cope with Sundowning at Home

Sundowning symptoms can be very challenging to manage at home. If your loved one has started displaying sundowning behaviors, here are a few tips that can help:
- Schedule activities, such as doctor’s appointments or shopping trips, for the morning or early afternoon when the patient is more likely to be alert.
- Encourage your loved one to follow a consistent routine of waking up, going to bed, and eating meals at the same time each day.
- Take notes about what happens just before a sundowning episode to see if you can identify triggers.
- Keep your home well-lit in the evening to reduce any shadows in the house, which may be confusing for patients.
- Find out what activities are soothing in the evening. Your loved one may enjoy looking at old photos or watching a favorite movie.
- Seek medical advice from your loved one’s doctors about possible therapies and medications, if needed.
- Make sure your loved one gets treatment for medical conditions, such as UTIs or incontinence, that are making sundowning symptoms worse.
- Ask for help when you need it. This could be asking family members to go shopping for you or using respite services to allow you and your family to have some time to rest.
- Make sure you eat a balanced diet and get plenty of rest.
- Join a caregiver support group. Meeting others in the same situation as you will give you a chance to share stories and keep you from feeling isolated.
- Consider seeking help from a mental health professional if you’re struggling with stress and anxiety.
Ways to Prevent Sundowning
Although it’s impossible to inhibit them completely, there are a few ways of reducing sundowning symptoms and limiting the severity of any episodes. Make sure your loved one with dementia:
- Gets enough rest at night.
- Avoids alcohol and caffeinated drinks after lunch. Instead, offer them decaf versions and alcohol-free beverages.
- Gets plenty of sunlight during the day.
- Exercises every day.
- Limits daytime naps to 20–30 minutes early in the afternoon. This will help the patient sleep better at night.
- Engages in some activities throughout the day, but be careful to avoid overstimulation. Activities should be those that the patient enjoys, such as visiting a favorite shop or going for a walk.
- Avoids having a large meal in the evening, as this can disrupt sleep patterns.
- Participates in relaxing activities in the evening, such as playing with a pet or listening to music. If watching television, make sure the volume is not too loud, as sudden noises can be distressing and trigger sundowning symptoms.
Ways to Manage Sundowning When Symptoms Occur
If, despite your efforts to prevent a sundowning episode, your loved one starts displaying symptoms, here are some ways to manage the situation:
- Use distraction techniques, such as moving the patient into a different room, offering them a snack or a drink, going out for a walk, or playing some music.
- Ask them what the problem is and listen to their answer. If possible, give them what they want. They may just be feeling lonely and want company or need to go to the toilet.
- Always talk to your loved one soothingly and use short sentences to avoid confusion. Also, if they like it, hold their hand or sit next to them. Don’t raise your voice, and don’t start an argument.
- Don’t physically restrain your loved one. If they want, let them pace back and forth (as long as it’s safe).
Neural Effects uses the latest evidence-based techniques to diagnose and help patients with dementia. We are located in Provo, Utah, and serve anyone in Salt Lake City or the Utah Valley area. We are in-network for most types of medical insurance. Schedule your evaluation today.
