Concussion treatment has changed dramatically over the past few years. For a long time, doctors advised concussed patients to stay in a dark room with limited mental and physical stimulation until symptoms disappeared.
Patients were told to avoid electronics, noise, and other activities, including exercise and socialization. Most patients recovered eventually, but students missed school and employees stayed home from work for an indefinite amount of time.
Today’s best practices for concussion recovery have evolved from this outdated advice of total rest. Modern research shows that introducing aerobic exercise and cognitive activities soon after a head injury — an approach known as active rehabilitation — can speed up recovery for both children and adults.
However, finding the correct intensity and timing for these activities can be tricky. Too much activity too soon can spike symptoms and impede the healing process. Meanwhile, too little activity can also delay recovery and put patients at a higher risk of developing long-term symptoms (a condition known as post-concussion syndrome or PCS).
The key is for patients to increase activity gradually and pay close attention to their body’s responses. This helps to strike the right balance of physical and cognitive activity at the right times during the healing process.
In this article, we’ll explain why active rehabilitation is important for individuals who’ve recently sustained a concussion. Then, we’ll walk through the types of activities that are safe to engage in and advice to consider as you progress through the following stages of recovery:
- Stage 1: The First 24–48 Hours
- Stage 2: Returning to Normal Activities (School, Work, and Screen Time)
- Stage 3: Monitoring Symptoms and Adding More Activities (Return to Sport)
- Stage 4: Getting Fully Back to Normal
Before we wrap up, we’ll also share:
- How we help patients recover from recent concussions at Neural Effects
- Advice for parents helping children recover from a concussion
- What you can do if symptoms last months and aren’t going away
If you live in Provo, Salt Lake City, or anywhere else in the Utah Valley area, we can help you recover from your concussion and reduce your chance of long-term symptoms. We are in-network for most types of medical insurance. Schedule your evaluation today.
The Importance of Active Rehabilitation to Promote Recovery After a Concussion

Cocooning — when patients stay in a dark room until symptoms dissipate — was developed based on studies in animals, which showed a period of high vulnerability in the brain immediately after the head injury. Cocooning was therefore developed to avoid putting excessive physical and cognitive demands on the brain and avoid any situation that could cause a second concussion with potentially devastating consequences.
However, studies show that strict cognitive and physical rest for too long after the concussion has no beneficial effect on patients when compared with no rest. Prolonged rest can slow recovery and aggravate some symptoms, such as fatigue, depression, anxiety, and physical deconditioning.
In contrast, moderate aerobic activity within a few days after a concussion accelerates recovery, and patients experience fewer symptoms. As such, doctors no longer recommend cocooning to treat patients. Instead, current treatments involve a short period of rest for 24–48 hours followed by a gradual increase in physical and cognitive activities.
Stage 1: Get Adequate Rest During the First 48 Hours After a Concussion

Resting immediately after a concussion is crucial because high physical and cognitive demands at this stage can worsen symptoms and delay recovery.
However, rest doesn’t mean you need to sit in a dark room all day and try not to think about anything. Instead, patients can still engage in simple activities as long as they’re not physically or cognitively demanding. For example, going for a short walk is fine but patients should avoid challenging chores such as paying bills or strenuous exercise.
In practical terms, physical rest means:
- No sports, physical activity, or workouts
- No strenuous house chores
- No strenuous leisure activities
- No sexual activity
- No driving
Cognitive rest may include:
- No work or school
- No homework
- No use of electronic devices (including phone, computer, tablet)
- No watching television
- No loud music
- No reading
- No playing musical instruments
- Limited socializing
What Can Patients Do During Rest?
Despite these limitations, there are plenty of ways to safely pass time during the first 48 hours. Some activities to consider include:
- Meditating
- Taking a relaxing bath
- Sleeping
- Having a relaxing massage or spa experience
- Listening to relaxing music, audiobooks, or TV (not too loud or for long periods)
- Helping with light household chores, such as folding laundry or setting the table
- Taking a short walk to get some fresh air
- Sitting outside in the garden
- Enjoying a quiet visit from a friend
- Playing quietly with a pet
- Going for a picnic in a quiet location
- Playing simple games (not on the computer or mobile phone)
- Engaging in simple arts and crafts or other creative activities
Stage 2: Gradually Return to Normal Activities
After this initial period of rest, patients should gradually start adding physical and cognitive activities back into their routines as concussion symptoms fade, including work and school. Engaging in physical exercise and doing cognitive tasks shortly after the injury can improve the chances of a full recovery.
In fact, one study showed that cognitive activities soon after a concussion increase heart rate variability, which shows that a part of the nervous system called the parasympathetic nervous system was activated by the task.
Why is this important? Briefly, the autonomic nervous system (ANS) contains two sections: the sympathetic nervous system (SNS), which controls the “fight-or-flight” response, and the parasympathetic nervous system (PNS), which controls the “rest-and-digest” response.
Under normal circumstances, the SNS and the PNS work together and are active at different times during the day depending on what the body needs. Concussions, however, change this balance, and many concussed patients are “stuck” with SNS all the time after their injury.
In the study that we mentioned earlier, the researchers showed that cognitive tasks after a concussion could trigger the PNS into action, which means that the brain is recovering (you can find out more about how the ANS is involved in brain injuries here).
The approach at this stage is to start with an easy activity for a short period of time, monitor symptoms, and then increase the level and intensity as patients feel better. If an activity is too much for you, go back to the previous activity level and try again in a few days. Symptoms may appear a few hours later or even the next day, not necessarily during the activity. Give your brain some time to adjust to the new activity, and don’t add more than two or three per day.
This needs to be a gradual process; trying to jump back into your normal pre-concussion activities is likely to trigger symptoms and delay your recovery.
Some activities you can try at this stage include:
- Enjoying some light reading
- Watching TV or playing on the computer for short periods (see below for more information)
- Listening to music, audiobooks, or podcasts
- Enjoying short visits from friends
- Engaging in brief periods of cognitive activities, such as school work or reading emails
- Engaging in light physical activity, such as going for a walk or spending a few minutes on a stationary bike
- Catching up with friends over the phone
- Engaging in creative activities, such as arts and crafts, painting, or drawing
- Engaging in self-care activities, such as going to a spa or getting a manicure
- Doing some light household chores
- Keeping a journal
- Cooking simple recipes
- Gardening
Some activities to avoid include:
- Attending school full-time
- Watching TV or playing on the computer for long periods
- Engaging in strenuous physical or cognitive activities, such as exams at school or multiple meetings at work
- Socializing in loud and noisy locations
Watching TV or Playing on the Computer
As patients may have to stay at home for longer than normal during this initial period, they’ll likely want to watch TV or play on the computer or mobile phone.
Until recently, the recommendation was to avoid the use of computer monitors, video games, and televisions until all symptoms resolved. This was typically part of the cocooning protocol discussed above. However, doctors now know there is no need to eliminate all screen time during recovery, as long as patients understand when to use these devices.
When it comes to screen time, consider the following:
- Try to avoid screens for the initial 48 hours after the injury.
- After this rest period, limit device usage to a few minutes during the first few days and gradually increase over time.
- Use devices as long as it doesn’t trigger or worsen symptoms. If a screen causes headaches, dizziness, or other symptoms, patients are advised to stop use or at least scale it back.
- Refrain from using these devices at night to ensure it doesn’t interfere with sleep patterns. If you’re having difficulties going to sleep, read some of our tips and tricks to ensure a good night’s sleep.
Returning to School
One of the advisable activities during this stage of recovery is a gradual return to school. Patients can begin by participating in low-stimulation activities such as reading or engaging in discussions with one or two people for up to 30 minutes.
It is generally not recommended to miss more than a week of school. Returning to school as soon as possible can be beneficial; extended absences may not only delay recovery but also make it more challenging to reintegrate into the school environment.
Return to school should be a gradual process, which may involve:
- Attending half-days or even just a few hours at first.
- Taking frequent breaks.
- Avoiding activities that need concentration, such as quizzes or tests.
- Having extra time for assignments, homework, quizzes, and tests.
- Having extra tutoring and help during class.
- Having extra resources including school-provided class notes and study guides.
- Making schoolwork up during vacation.
- Wearing sunglasses due to light sensitivity.
Returning to Work
When returning to work, patients should follow a similar process to returning to school. Return to work only when the majority of symptoms have diminished and physical and cognitive endurance can be maintained for a certain period. It depends on the type of job you do, but as a general guide, you need to be able to concentrate or engage in physical or cognitive activities for about 2 hours.
A gradual return to work safely may include:
- Working from home at first.
- Starting on reduced hours or lighter workload then gradually increasing back to normal activities.
- Working in a quiet space to help patients focus on their tasks.
- Taking plenty of break times throughout the day (this allows patients to remove themselves from a busy and stimulating environment and go to a quieter space).
- Breaking down large tasks you have to do into smaller chunks.
Stage 3: Monitor Symptoms and Add More Activities

As symptoms dissipate in the days and weeks following the concussion, patients can gradually add more cognitive and physical activities, but they need to be careful to monitor symptoms and avoid overexertion.
A study found that high school athletes who started high levels of activity shortly after their concussion performed worse on cognitive activities than those who started gradually and engaged in mild to moderate levels at first.
Knowing When to Stop
Patients need to learn to listen to their bodies and understand when it’s time to stop if they’re experiencing too many symptoms. Our advice is to follow the rule of three:
- If you notice three symptoms worsening (such as brain fog, headache, and dizziness), then it’s time to take a break.
- If the severity of a single symptom increases by three on a six-point scale (for example, your headache increases from a 1 to a 4), then it’s time to stop.
- If you’re just experiencing one or two very mild symptoms — such as your vision is a bit blurred and your brain feels vaguely foggy — then it’s safe to continue your activity. In fact, when patients experience mild symptoms, it means that they’re pushing themselves in exactly the right amount to promote a faster recovery.
Avoiding a Second Concussion
In addition, patients should avoid activities that put them at risk for another concussion. If you suffer a second concussion before the first has a chance to heal, you may develop Second Impact Syndrome (SIS), which may be fatal or cause permanent disabilities. Examples of activities that may cause this include:
- Contact sports (such as football, hockey, or soccer)
- Dangerous sports (such as climbing)
- Riding a bicycle or a motorbike without a helmet
- High-risk jobs (such as mining or construction)
Adding In Activities Safely and Appropriately
Activities that you may begin adding in at this stage include:
- Progressing through the return to school/work protocol
- Starting a return-to-play protocol (see below)
- Going out with friends
- Gradually increasing in sports and recreational activities
Activities to avoid at this stage include:
- Engaging in highly demanding sports or physical activity (patients should follow the return to play protocol without jumping steps)
- Engaging in highly demanding cognitive activities (such as too many tests at school or heavy workload)
Returning to Sport
Athletes may be eager to get back to training, but it’s important to wait until patients are symptom-free before they attempt to play sports. Healthcare providers typically consider that patients are ready to resume training when they are:
- Free of concussion symptoms for at least 24 hours
- Off any medications started for concussion symptoms (which may mask symptoms)
- Attending school/work and tolerating a full day of academic/work activities
Similar to the process of going back to school or work, getting back into sports should be gradual. The Return to Play Program outlines six stages to guide athletes and coaches to determine when patients are ready to move on to the next stage. Each stage should last at least 24 hours before moving on to the next:
- Stage 1: Patients are back to their regular daily activities, such as attending school or work (as described above).
- Stage 2: As symptoms start to subside, athletes can do light aerobic activity, such as 10 minutes of walking or stationary biking as long as it doesn’t aggravate symptoms too much (see above for knowing when to stop). The aim is to increase the athlete’s heart rate and stimulate blood flow to the brain.
- Stage 3: When athletes are symptom-free, they can increase aerobic activity and add light resistance training, as well as low-risk activities like dribbling a basketball or playing catch. Patients can do moderate jogging, brief running, moderate-intensity stationary biking, and moderate-intensity weightlifting (less time and/or less weight from their typical routine).
- Stage 4: Athletes can add heavy non-contact physical activity, such as sprinting/running, high-intensity stationary biking, regular weightlifting routine, and non-contact drills specific to their sport.
- Stage 5: With supervision and regular symptom checks, athletes can resume full-contact training drills (if appropriate for the sport).
- Stage 6: Athletes are cleared to return to the sport and normal gameplay.
If patients experience symptoms at any stage, they should go back to the previous stage and only progress to the next level after 24 hours of symptom-free rest.
Stage 4: Getting Fully Back to Normal

Most patients return to normal within a few days or weeks at most. When protocols to return to school/work and sports are completed, patients shouldn’t be experiencing any symptoms caused by their concussion. At this stage, they can engage freely in all their pre-concussion activities without any restrictions.
Usually, a physician will consider patients fully recovered when:
- They have no symptoms (or very minor symptoms), even after an intense exercise session.
- They’ve regained all their physical and cognitive skills.
- They feel back to normal.
To sum up, the activities to do and activities to avoid at each of the recovery stages we’ve discussed so far include the following:
| Activities allowed | Activities to avoid | |
| 24–48 hours after concussion | ‣ Meditating ‣ Taking a relaxing bath ‣ Sleeping ‣ Having a relaxing massage or spa experience ‣ Listening to relaxing music, audiobooks or TV ‣ Helping with light household chores, such as folding laundry, setting the table ‣ Taking a short walk to get some fresh air ‣ Sitting outside in the garden ‣ Enjoying a quiet visit from a friend ‣ Playing quietly with a pet ‣ Going for a picnic in a quiet location ‣ Playing simple games (not on the computer or mobile phone) ‣ Engaging in simple arts and crafts or other creative activities | ‣ Physical activity ‣ Strenuous house chores ‣ Strenuous leisure activities ‣ Sexual activity ‣ Driving ‣ Work or school ‣ Homework ‣ Use of electronic devices, including phone, computer, and tablet ‣ Television ‣ Loud music ‣ Reading ‣ Playing musical instruments ‣ Socializing |
| Gradually returning to normal activities | ‣ Enjoying some light reading ‣ Watching TV or playing on the computer for short periods ‣ Listening to music, audiobooks or podcasts ‣ Enjoying short visits from friends ‣ Engaging in brief periods of cognitive activities, such as school work or reading emails ‣ Engaging in light physical activity, such as going for a walk or spending a few minutes on a stationary bike ‣ Catching up with friends on the phone ‣ Engaging in creative activities, such as arts and crafts, painting, or drawing ‣ Engaging in self-care activities, such as going to a spa or a manicure ‣ Doing some light household chores ‣ Keeping a journal ‣ Cooking simple recipes ‣ Gardening | ‣ Attending school full-time ‣ Watching TV or playing on the computer for long periods ‣ Engaging in strenuous physical or cognitive activities, such as exams at school or multiple meetings at work ‣ Socializing in loud and noisy locations ‣ Engaging in large group activities |
| Monitoring symptoms and adding more activities | ‣ Progressing through the return to school/ work protocol ‣ Starting return to play protocol ‣ Going out with friends ‣ Gradually increase in sports and recreational activities if not started already, starting treatment at Neural Effects | ‣ Engaging in highly demanding sports or physical activity (patients should follow the return to play protocol without jumping steps) ‣ Engaging in highly demanding cognitive activities (such as too many tests at school or heavy workload) |
| Getting fully back to normal | ‣ All | ‣ None |
How We Help Patients Recover From Recent Concussions at Neural Effects
By following the protocol discussed throughout this post, patients can make significant progress toward healing. However, you may also consider getting professional support through a concussion clinic that specializes in helping individuals recover from acute concussions.
Neural Effects is one of the few concussion clinics in the U.S. that combines both physical and cognitive therapy to treat concussed patients. This combination helps individuals rebuild neural pathways that were disrupted by their concussions, which in turn can help them reduce symptoms and recover faster.

Before treatment starts, patients go through a detailed medical evaluation to find out how exactly the concussion affected their bodies. Our therapists want to get a complete picture of the patient’s situation, including any pre-existing conditions and what concussion symptoms they’re experiencing.
During this assessment, patients complete the following:
- Discuss their medical history with a member of our team: This is vital to get information about any pre-existing health conditions that might affect the patient’s recovery.
- Discuss the results from imaging scans, such as CT scans, MRIs, or X-rays: While these scans can’t diagnose a concussion, they are useful to check for skull fractures or to look for signs of bleeding in the brain. For patients who haven’t had any scans done, our team can decide if they’re needed. We have an X-ray machine and an MRI machine on-site, so we can get those done quickly if we believe they are necessary.
- Cranial nerve exam: This test assesses the twelve cranial nerves that control movement and senses in the head, such as eye movements, facial muscles, jaw movements, and others.
- Cervical spine exam: During this exam, our therapists check your spine, neck, arms, and hands to identify fractures or herniated discs. We also measure muscle strength and evaluate whether strength is the same on both sides of the body. If we find any signs of a neck or spine injury that require additional imaging or a referral to a specialist, we can arrange for that.
- Balance Error Scoring System (BESS) test: This includes a series of simple balance exercises done with closed eyes. It is often used to evaluate athletes after a potential concussion during a game. The results of this test help us determine which areas to target during therapy.
- Visual assessment: Patients are assessed for visual problems, such as problems with focus or double vision. These symptoms are common after a brain injury, including changes to peripheral vision, depth perception, and ability to focus.
Once this examination is complete, our therapists tailor therapy for each patient based on their specific symptoms. For example, if patients struggle with dizziness and balance problems, our therapists will emphasize vestibular exercises; if most of the symptoms are vision-related, our therapists will spend some time doing eye-related exercises.
In general, patient sessions follow a similar structure, including:
- Post-concussion Symptom Scale
- Physical therapy
- Vestibular and vision therapy
- Neuromuscular and cognitive therapy
- Breathing techniques
- Activities to do at home
Post-Concussion Symptom Scale
We start and end every therapy session with the post-concussion symptom scale. Patients list their symptoms against a symptom checklist and rate them on a scale from zero (no symptoms) to six (the worst possible) in terms of severity. This allows us to monitor symptoms and track progress. It also guides our decisions about your therapy.
Physical Therapy
Sessions start with a short session of physical exercise, typically on a treadmill or stationary bike. This increases blood flow to the brain and triggers a mechanism in the brain called a post-exercise cognitive boost (PECB) — a vital component of the healing process. PECB sparks the production of neurochemicals that stimulate healing, including one called brain-derived neurotrophic factor (BDNF) which helps the brain learn better and helps patients benefit from subsequent therapy.
Our therapists are trained to ensure patients exercise enough to raise their heart rate, which improves blood flow to the brain — crucial for the areas affected by the concussion — but not so much that it triggers symptoms. This is known as exercising at the sub-symptom threshold.
Vestibular and Vision Therapy
After a concussion, it’s common for patients to experience dizziness, nausea, and vertigo, as well as problems focusing, double vision, and other eye-related symptoms. These symptoms can result from disrupted communication between the eyes (vision), ears (vestibular), and the brain.
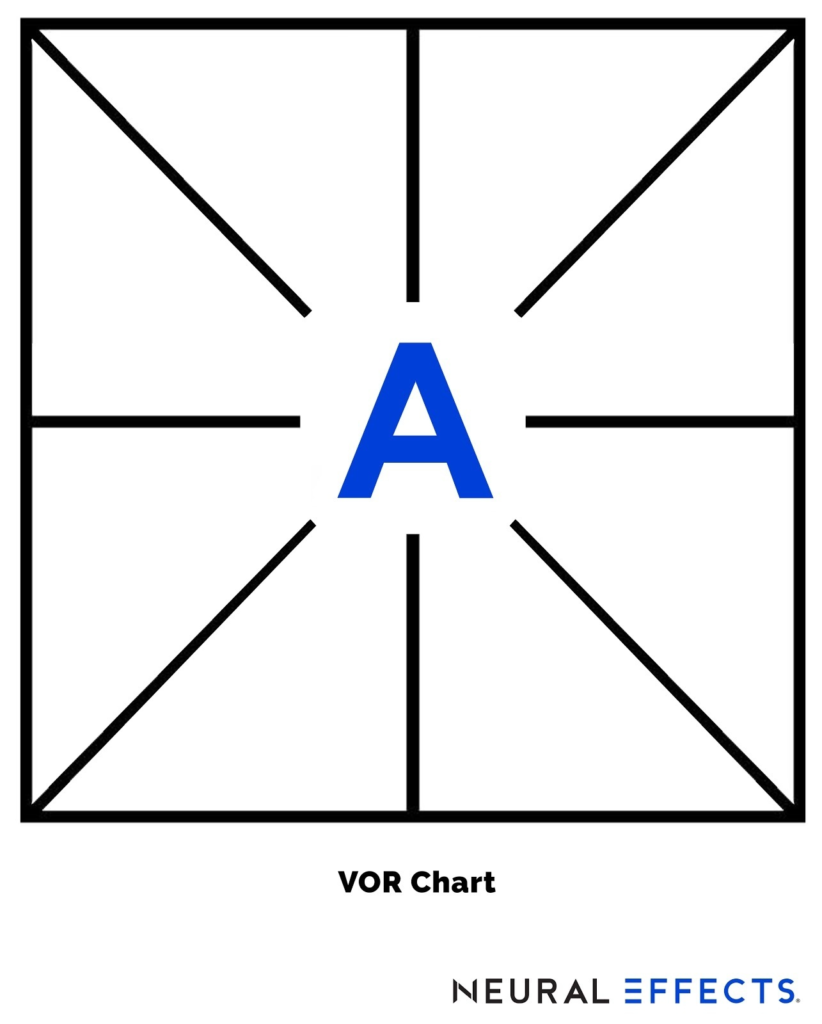
Ocular and vestibular rehabilitation are designed to get these systems working together again. Our therapists can use a variety of activities, such as:
- Exercising with the Vestibular Ocular Reflex (VOR) chart. This chart is placed on a wall at eye level. It has a large letter A in the middle with lines running from the A in all directions. Patients need to focus on the A and then move their heads along the lines, back and forth.
- Performing Brock String exercises. Patients use a string with beads spaced at equal distances to help retrain the eyes to work together to focus properly.
Neuromuscular and Cognitive Therapy
Neuromuscular therapy can be used to treat balance, multisensory, and cognitive issues caused by the concussion.
Examples of activities that our therapists can do during their sessions include:
- Balancing on a Bosu ball while playing a memory word game.
- Hitting targets in random patterns to improve reaction time.
- Throwing color-coded balls back and forth while thinking of a word for each letter of the alphabet for a particular category. For example, names of cities or types of animals.
- These exercises are designed to get the brain and body working together again. Throughout these exercises, therapists monitor the patient’s symptoms and make adjustments as needed. Patients may also engage in purely cognitive activities, including memorizing pictures, solving a logic puzzle, recognizing patterns, and more.
Breathing Techniques
Patients also learn various breathing techniques to help them relax and recover from exercise without triggering symptoms. Patients can continue to use many of these breathing techniques at home after treatment to help during their recovery.
Activities to do at home
After each session, patients receive a series of activities to do at home. Typically, this consists of about an hour of aerobic exercise, cognitive activities, breathing exercises, and rest. Doing this homework diligently will accelerate your recovery.
If you live in Provo, Salt Lake City, or anywhere else in the Utah Valley area, we can help you recover from your concussion and reduce your chance of long-term symptoms. We are in-network for most types of medical insurance. Schedule your evaluation today.
Advice for Parents: Helping Your Children Recover From a Concussion

With a few adaptations, everything we’ve described so far also applies to children, adolescents, and teenagers. Here is some advice specific to parents:
Don’t restrict your child after a concussion
We understand that your first instinct as a parent is to protect your child after a concussion. You may want to keep your child away from light, noise, and any kind of activity. But, as we’ve explained earlier, this may actually delay their recovery.
Instead, encourage your child to take a day or two of rest and then slowly introduce physical and cognitive activities. One suggestion is to start with simple school work and light aerobic activities such as going for a short walk or riding a stationary bike. If your child’s symptoms don’t worsen during an activity, then it’s OK to continue. If symptoms worsen, they should cut back on that activity and try again a few days later. Don’t allow your child to stay in their bedroom all day doing nothing.
Don’t rush going back to normal
On the other hand, if your child is keen to go back to their normal life too soon, you need to help them follow a gradual process to introduce new activities. If your child gets back too quickly, they increase their chances of aggravating symptoms or sustaining another injury.
Challenge the brain
Cognitive activities “force” the brain to use neural pathways that may have been affected by concussion, thereby helping it recover. Anything that stimulates the brain can be useful, from board games to homework. Board games, mazes, crossword puzzles, and sudoku are all good options, but you can find a complete list here.
As we’ve described earlier, gradually increasing school attendance also helps.
Pay attention to your child’s mental health
It’s common for children to become frustrated and anxious while they recover from a concussion due to the limitations they experience in learning, social activities, and sports. It’s critical to monitor your child’s mood and offer support if necessary.
Consider seeking treatment at a concussion clinic
If you want to improve the chances that your child will recover fully after their head injury, consider seeking treatment at a concussion clinic.
This article can help you learn what to look for in a concussion clinic, and how to find one near you.
What You Can Do If Symptoms Aren’t Going Away
While most patients see symptoms resolve after their concussion, some patients continue to experience persistent symptoms for months or even years. This condition is called post-concussion syndrome (PCS) and it can be more challenging to treat than an acute concussion.
If you’re experiencing lingering symptoms after your concussion, our sister company, Cognitive FX, specializes in treating this condition. They use state-of-the-art brain imaging techniques to precisely identify the parts of the brain affected by the head injury. Following diagnosis, they provide a tailored combination of exercise and multidisciplinary therapies to address your specific symptoms.
You can learn more about their service here.
