Your brain controls the way you think, what you remember, how you solve problems, and much more. These cognitive abilities influence how well you can do your everyday tasks and determine if you can live independently.
Some changes in these cognitive abilities are normal as people get older. For example, older adults may become slower to recall names or forget where they put the car keys. However, if you’ve noticed your memory lapses getting more frequent or you become frustrated that you struggle to find the right words, you may have Mild Cognitive Impairment (MCI).
Surprisingly, this condition is not as well-known as dementia. In fact, a recent survey showed that fewer than one in five Americans are familiar with MCI and only four in 10 would actually talk to their doctor right away when experiencing symptoms of MCI.
Sometimes, people confuse MCI with early-stage dementia. The two are not the same. MCI does not always develop into dementia and is much more responsive to treatment. That’s why it’s so important to seek medical advice if you experience any signs of MCI. Early intervention can make a big difference in your ability to live independently and to continue doing the things you love.
In this post, we’ll explain…
- What the signs and symptoms of mild cognitive impairment are (and how to tell them apart from normal aging)
- What causes MCI
- Who is more likely to develop MCI
- How MCI is diagnosed
- What the best treatment options are for MCI
- What you can start doing at home to combat MCI
Neural Effects uses the latest evidence-based techniques to diagnose and help dementia patients. We are located in Provo, Utah, and serve anyone in Salt Lake City or the Utah Valley area. We are in network for most types of medical insurance. Schedule your evaluation today.
What Are the Signs and Symptoms of Mild Cognitive Impairment?

As you get older, it’s important to understand the differences between normal age-related memory issues and conditions like mild cognitive impairment (MCI) and dementia.
MCI causes changes in memory, thinking, and other cognitive skills that are serious enough to be noticed by the patient or their loved ones. Patients may need a little help with more demanding tasks, such as paying bills or managing medication, but it doesn’t cause major problems with their daily life. If there is a significant impact on everyday activities, it’s more likely to be dementia.
MCI is classified as one of two types, based on a person’s symptoms:
- Amnestic MCI, where patients predominantly experience memory loss, such as forgetting conversations or misplacing their house keys.
- Nonamnestic MCI, where patients experience other cognitive issues, such as impairments in language, visuospatial abilities, or executive function. In this case, patients may struggle to follow a conversation, find their way around in a familiar location, or complete complex tasks such as paying all the bills on time.
Patients may experience one or more of the following signs of MCI:
- Memory problems (forgetfulness about recent events, repeating the same question, etc.)
- Struggles with reasoning and problem-solving
- Problems with attention (being easily distracted from tasks, losing focus on what someone is saying, struggling to begin a task, etc.)
- Language deficiencies (taking longer than usual to find the right word, etc.)
- Changes to visual depth perception (struggling to interpret an object in three dimensions, judge distances, or navigate stairs, for example)
- Emotional symptoms (depression, apathy, irritability, anxiety, agitation, etc.)
- Sleep disturbances (trouble falling asleep, trouble staying asleep, not feeling well rested, etc.)
Does MCI Always Develop Into Dementia?
Although some symptoms are similar, there is a marked difference between MCI and forms of dementia, such as Alzheimer’s disease or vascular dementia. In addition, an MCI diagnosis does not necessarily mean that the patient will develop dementia. In fact, only about 10% to 15% of MCI patients go on to develop dementia each year, and about one-third of MCI patients develop dementia within five years. Some people with MCI revert to normal cognition or do not suffer any additional cognitive decline as they get older.
Identifying which MCI patients are more likely to develop dementia is a major goal of current research. Identifying cognitive issues that result from normal aging, those associated with MCI, and those present in patients that will develop some form of dementia is critical to help patients, their families, and their doctors prepare for future treatment and care.
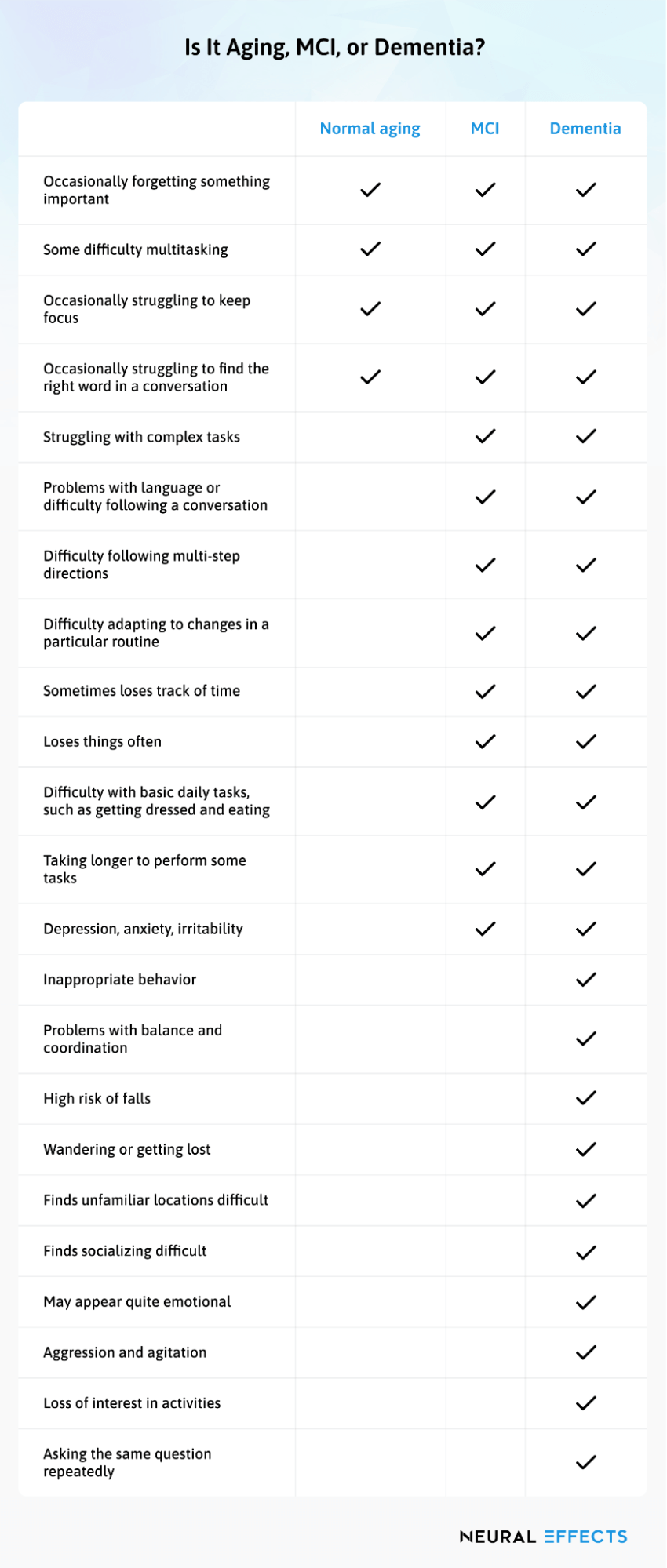
While this chart is NOT a substitute for visiting a health care professional and does not constitute medical advice, it may help you understand the difference between normal signs of aging, MCI, and dementia.
Is It Aging, MCI, or Dementia?
| Aging | MCI | Dementia | |
| Occasionally forgetting something important | ✔ | ✔ | ✔ |
| Some difficulty multitasking | ✔ | ✔ | ✔ |
| Occasionally struggling to keep focus | ✔ | ✔ | ✔ |
| Occasionally struggling to find the right word in a conversation | ✔ | ✔ | ✔ |
| Struggling with complex tasks | ✔ | ✔ | |
| Problems with language or difficulty following a conversation | ✔ | ✔ | |
| Difficulty following multi-step directions | ✔ | ✔ | |
| Difficulty adapting to changes in a particular routine | ✔ | ✔ | |
| Sometimes loses track of time | ✔ | ✔ | |
| Loses things often | ✔ | ✔ | |
| Difficulty with basic daily tasks, such as getting dressed and eating | ✔ | ✔ | |
| Taking longer to perform some tasks | ✔ | ✔ | |
| Depression, anxiety, irritability | ✔ | ✔ | |
| Inappropriate behavior | ✔ | ||
| Problems with balance and coordination | ✔ | ||
| High risk of falls | ✔ | ||
| Wandering or getting lost | ✔ | ||
| Finds unfamiliar locations difficult | ✔ | ||
| Finds socializing difficult | ✔ | ||
| May appear quite emotional | ✔ | ||
| Aggression and agitation | ✔ | ||
| Loss of interest in activities | ✔ | ||
| Asking the same question repeatedly | ✔ |
What Are the Causes of MCI?
In some patients, MCI symptoms stem from a treatable medical condition. Symptoms may arise from conditions such as a traumatic brain injury, stroke, side effects from medication, poor eyesight or hearing, vitamin deficiency, or thyroid deficiencies. They could also come from mental health struggles such as depression, anxiety, or stress.
In other patients, MCI is the consequence of changes that occur in the brain. These brain changes may not be reversible and, in time, could cause dementia. If the brain changes involve the presence of biomarkers showing early stages of Alzheimer’s pathophysiology, including presence of beta-amyloid plaques and atrophy of the hippocampus, then it is called MCI due to Alzheimer’s. These MCI patients are at risk of developing some types of dementia.
What Are the Risk Factors for Developing MCI?

Your chances of developing MCI are dependent on many factors, some of which are out of your control. Elderly patients are more at risk of cognitive changes. Genetics also plays a role, so it’s worth considering whether you have any family members who have dementia or other neurodegenerative disorders.
However, there are also risk factors that you can control. Treating these conditions decreases your chances of developing MCI or slows down progression of the disease if you already have MCI. Some of these factors include:
- Poor cardiovascular health. Patients with heart conditions and hypertension are at increased risk of cognitive impairment. This could be because heart disease and dementia share common risk factors or because cardiac complications can directly affect cognitive health.
- Smoking or excessive drinking: Smoking or excessive drinking can cause various physical and mental health complications, including an increased risk of cognitive decline and MCI.
- Elevated cholesterol. High total blood cholesterol may increase your risk of cognitive decline.
- Sleep problems. Patients who struggle with conditions that affect their sleep, such as insomnia or waking up frequently during the night, are more prone to developing MCI.
- Lack of mental and social engagement. Your brain needs interactions with other people and cognitive stimulation. Long periods of isolation may increase your risk of MCI.
- Sedentary lifestyle and lack of exercise. Engaging in regular physical activity improves cognitive function and helps you manage other risk factors, such as high blood pressure and cardiovascular health.
- Diabetes. This condition increases your risk of MCI due to its effect on the vascular system.
- Untreated mental health issues. Untreated mental health conditions such as depression and anxiety put you at a higher risk of developing MCI.
- Multiple chronic conditions. Having multiple chronic conditions, such as arthritis, chronic lung disease, cataracts, stroke, and hearing problems, can increase your risk of MCI.
How Do You Receive a Diagnosis of MCI?

In order to determine whether or not you have MCI, your doctor may ask for the following:
- A detailed medical history, including current symptoms, previous medical conditions, and a family history of significant memory problems or dementia.
- Assessment of how you carry out daily activities.
- Input from a family member or a close friend to add important information about how cognitive function may have changed for you.
- An evaluation of cognitive skills using tests to assess memory, planning, judgment, the ability to understand visual information, and other key thinking skills.
- A neurological examination to assess reflexes, movement, coordination, balance, and senses.
- A neuropsychological test to assess depression and anxiety symptoms.
- Several laboratory tests including blood tests and brain imaging, especially if the doctor suspects other medical conditions.
All the tests described above will provide valuable clues about whether you have MCI. That said, there is no one single test that can definitely confirm an MCI diagnosis. An MCI diagnosis represents your doctor’s best judgment, taking into account all the results from testing.
If you receive an MCI diagnosis, maintain regular appointments with your doctor to monitor your condition and detect any transition into dementia. An early diagnosis and subsequent follow-ups means you can have access to support and treatment as needed.
What Are the Current Treatment Options for Mild Cognitive Impairment?

There are currently no FDA-approved prescription drugs to treat MCI. It was hoped that Donepezil — used in Alzheimer’s patients — could help with MCI symptoms, but clinical trials failed to find a clear benefit for patients.
There are currently some meds undergoing clinical trials. The most promising is called Lecanemab, which showed positive results for patients living with MCI and early Alzheimer’s disease. In July 2022, the FDA accepted an application for the accelerated approval pathway and granted Priority Review for Lecanemab.
Treatment for MCI also involves treating all the conditions which increase your risk of further cognitive decline. If you have a heart condition, high blood pressure, blood clots, depression, anxiety, or high cholesterol, for example, you may need to treat those conditions with lifestyle changes, therapy, medications, or some combination thereof. Just be aware that the side effects of certain medications can actually contribute to MCI symptoms, so patients and prescribing physicians need to keep a close eye on symptoms after any medication change.
One of the best approaches to MCI treatment is physical and cognitive therapy, which we use at Neural Effects because it is so effective.
Treatment at Neural Effects

We believe the best way to delay progression of symptoms and minimize your chances of developing dementia is with a combination of physical exercise and cognitive activities.
Before treatment, each patient goes through a neuropsychological exam (also called a neurocognitive evaluation) to find out what kind of cognitive problems they have. This exam includes tests to assess attention, memory, executive function, and other cognitive skills. We also assess patients for symptoms related to depression and anxiety.
Once the exam is completed, patients meet with our team to decide on a treatment approach.
If you decide to start treatment with us, we provide a combination of physical exercise and a range of therapies (physical therapy, cognitive therapy, neuromuscular therapy, occupational therapy, and more) based on the problems identified during the initial exam. Activities we use in treatment are designed to improve memory, attention, executive function, thinking skills, language, vision, and more.
This combination is so effective in part because physical exercise triggers a phenomenon in the brain called the post-exercise cognitive boost (PECB). PECB involves the release of an important compound called brain-derived neurotrophic factor (BDNF), which in turn makes the brain more receptive to building new connections during therapy. As a result, the brain is more “flexible” and better able to benefit from therapy after exercise.
You can attend your sessions with a family member or caregiver so that they can learn the exercises and help you at home. At the end of each session, our therapist will give you exercises to do at home. This is an important part of treatment; completing the exercises at home will significantly improve the overall effect of therapy.
Neural Effects is located in Provo, Utah and serves anyone in the Salt Lake City or the Utah Valley area. We’re in network for most types of medical insurance. Contact us today to schedule your evaluation.
What You Can Do at Home

Lifestyle adjustments can give you more control over the progression of MCI symptoms, help you cope with activities of daily living (ADLs), and reduce the risk of developing dementia. Here are the most important ones:
Engage in regular exercise
Exercise remains one of the best things you can do to slow down progression of MCI symptoms. A study following almost 250,000 MCI patients over six years found that even modest amounts of exercise can help delay cognitive decline. Patients who only started exercising after their MCI diagnosis still benefited from it.
Your workout does not have to be extreme. If you can cope, it should be challenging enough to increase your heart rate, but not to the point that you find yourself out of breath and exhausted. Try to engage in physical activity for about 30 minutes a day for five days a week.
Challenge your brain
Keeping your brain active and learning new skills is another way to delay progression of the disease. Studies show that cognitive stimulation can improve memory, attention, mental flexibility, processing speed, and executive function in MCI patients.
Rekindle an old hobby, learn a new language, or play board games with your friends. Find something you enjoy doing that requires you to use your cognitive skills. You don’t have to choose something particularly difficult, just something you find engaging and interesting enough to nurture your brain.
Keep socially active
Your relationships with friends and family don’t just help you feel better. They also protect your brain. Maintain regular interactions with others; this can be through video chatting with family members, a regular meal out with friends, or daily conversations with your neighbors.
Follow a healthy diet
Following a balanced and healthy diet can also protect cognitive function.
For example, the MIND diet — a diet specifically designed to protect brain function — emphasizes the consumption of leafy green vegetables, berries, legumes, fish, nuts, and whole grains while limiting the consumption of butter, cheese, and red meat. This diet can slow down age-related cognitive decline and reduce the risk of Alzheimer’s disease.
Follow good sleep habits
Sleep disturbances are common in MCI patients, but addressing these problems goes a long way in preventing cognitive decline. Here are some tips to help you get consistent, good-quality sleep:
- Keep a consistent bedtime routine, even during weekends and holidays.
- Avoid caffeinated drinks and alcohol late in the day.
- Limit daytime naps to 15-20 minutes.
- Do something relaxing before bedtime (taking a warm bath, reading a book, etc.).
- Avoid using your phone before bed.
Neural Effects uses the latest evidence-based techniques to diagnose and help dementia patients. We are located in Provo, Utah, and serve anyone in Salt Lake City or the Utah Valley area. We are in network for most types of medical insurance. Schedule your evaluation today.