A dementia diagnosis is never easy to hear, whether you’re the patient or one of their loved ones. If you’re anxious about the future, that’s normal — it can take time to learn what your loved one needs and how best to help them as they navigate this disease.
Since dementia patients are often helped by a combination of medications, therapy, and lifestyle adjustments, we’ve created this guide to review what’s available and how and when you might use them.
You can read the whole guide or skip to the following sections:
- Medications available for dementia patients
- Non-pharmacological approaches (therapy)
- Dementia treatment at Neural Effects
- Ways to help at home with lifestyle adjustments
Neural Effects uses the latest evidence-based techniques to diagnose and help dementia patients. We are located in Provo, Utah, and serve anyone in Salt Lake City or the Utah Valley area. We are in network for most types of medical insurance. Schedule your evaluation today.
Medications for Dementia

If you’re caring for a loved one with dementia, it helps to understand what type of medications exist for dementia and when doctors prescribe them. It will also help you advocate for your loved one when talking with doctors about treatment options.
Prescription dementia medications exist to lessen symptoms and help the patient maintain quality of life for as long as possible. Many dementia patients find them helpful; however, each patient is unique. It’s important to monitor their symptoms and to weigh any side effects against the benefits they experience.
Keep in mind that not every medication is appropriate for every type of dementia. Some medications helpful for Alzheimer’s disease (AD) may not be helpful to a patient with frontotemporal dementia, for example.
Doctors can use prescription drugs to:
- Slow down disease progression
- Treat dementia symptoms
- Treat sleep disturbances
- Treat depression and anxiety
- Treat challenging behavior
Here’s a closer look at each.
Drugs to Slow Down Disease Progression
Until recently, there was no way to slow down progression of Alzheimer’s disease using prescription drugs. However, in June of 2021, the FDA approved a new therapeutic drug called Aducanumab (Brand name: Aduhelm).
This drug targets beta-amyloid, a protein that forms in the brain and eventually starts accumulating into clumps, which are called plaques. These plaques block communication between neurons and activate the immune system to trigger an inflammatory response and kill disabled nerve cells.
Aducanumab is the first therapy to remove these plaques from the brain. Participants in one clinical trial who received aducanumab experienced an improvement on paper in memory and thinking skills, but did not report any noticeable improvements in day-to-day life.
Patients considering Aducanumab should be aware of the controversy surrounding its FDA approval. (Note that it still has not been approved for use in Europe.) There is no definitive evidence that removing the plaques produces symptom improvement; further research is needed, especially since it has only been tested in patients with mild cognitive impairment (MCI) and early stage dementia.
Meanwhile, Aducanumab has several downsides: it’s expensive; it must be taken by IV; and it has side effects including brain swelling, small brain bleeds, headaches, increased risk of falls, diarrhea, and confusion. Medical professionals are split on whether patients should have access to the drug. Some believe the questionable benefit is not worth the high cost and side effects. Others believe it’s still a better option than doing nothing.
Drugs to Treat Dementia Symptoms
Most dementia medications control or stabilize symptoms, at least for a time.
One example is cholinesterase inhibitors (such as Donepezil, Rivastigmine, and Galantamine).These drugs are often prescribed to treat symptoms related to memory, thinking, language, and other cognitive functions. They work by preventing an enzyme called acetylcholinesterase from breaking down acetylcholine in the brain, which helps nerve cells communicate with each other. As a result, there is a higher concentration of acetylcholine in the brain, which may lead to better communication between nerve cells.
Cholinesterase inhibitors are commonly used to treat patients with Alzheimer’s disease, but there is some evidence that these medicines can also help patients with Lewy bodies and Parkinson’s disease, as well as some patients with mixed dementia.
Only about half of patients who take a cholinesterase inhibitor feel some benefits. Unfortunately, there is no way to know in advance whether the medication will help a patient or not. When the treatment helps, patients experience symptom improvement for up to 12 months, but this effect wears off over time.
These drugs are generally well-tolerated, but side effects may include nausea, vomiting, loss of appetite, increased frequency of bowel movements, and urinary incontinence.
A second class of dementia medications includes glutamate regulators (Memantine). These drugs are also prescribed to improve memory, attention, and language, and are suitable for those who cannot take, or are unable to tolerate, acetylcholinesterase inhibitors.
As the name suggests, they work by regulating the activity of glutamate, a substance that helps the brain process information. Glutamate is important for normal brain function, but when nerve cells are damaged or degrading, they can release too much glutamate. As a result, that glutamate can cause hyperexcitability of the cells and further damage. Memantine protects nerve cells by blocking glutamate from getting to glutamate receptors.
Most people can take memantine without too many side effects. The most common side effects include dizziness, headaches, and tiredness. Some patients may also experience raised blood pressure and constipation.
Drugs to Treat Sleep Disturbances
Persistent waking or problems falling asleep at night can cause many difficulties for dementia patients. To make matters worse, some drugs prescribed to treat other symptoms can cause patients to feel sleepy during the day, but interfere with restful sleep at night.
Sleep medication for dementia patients should be used as a last resort, but it can be useful for some patients. These hypnotics are sometimes used only when the patient feels they need a good night’s sleep, rather than taking them every night, which may cause them to become completely reliant on the medication to sleep.
Fortunately, there are ways to help dementia patients sleep better more consistently (discussed later in this post).
Drugs for Depression and Anxiety
Symptoms of anxiety and depression are common in patients with dementia. Non-drug interventions such as regular exercise can be very useful; if you’re worried about medication side effects, it’s a good starting option. For patients who don’t respond well to other interventions, antidepressants may help improve mood, control irritability, and reduce anxiety. It may take a few weeks or months for patients to feel any benefits, so it’s important that they take the medication consistently.
The most common antidepressant drugs used in dementia patients are known as selective serotonin reuptake inhibitors (SSRIs). These are typically well tolerated by patients with dementia, but some may experience headaches and nausea, especially during the first two weeks of treatment.
Antidepressants are another source of controversy in dementia treatment. Some studies show an increased risk of developing dementia due to SSRIs or tricyclic antidepressants, and other researchers argue that antidepressants should help to alleviate dementia. At this point, it isn’t clear whether they worsen patients’ condition or not. In addition, the long-term benefit of antidepressants to elderly patients is not well established. (Most studies do not follow up with patients much beyond one year.) Thus, patients and their family caregivers should discuss the benefits and risks carefully with their doctors before starting their use.
Drugs to Treat Challenging Behavior
Some patients with dementia develop behavioral and psychological symptoms, including increased agitation, anxiety, and aggression. These changes can be very stressful both for the patients and their carers. Antipsychotic medication, such as risperidone or haloperidol, is sometimes prescribed for those showing persistent aggression or extreme distress.
Managing Your Loved One’s Medications
If your loved one needs to start meds for dementia, they may need your help but may want to feel as though they’re in charge of their medication. Here are some ways in which you can help:
- Get a pill organizer box that you fill up with the correct medication once a week. Make sure you store the bottles of labeled medications somewhere safe to avoid accidental ingestion.
- Follow a daily routine to help them remember to take their medicine. It’s easier if you fit medication around their normal activities, like meal times.
- Set an alarm to help them remember to take their medicine when you can’t be there.
It’s good practice to review medication every six to twelve months. Your loved one may be able to stop taking medications that are no longer effective. That would mean fewer overall medications and a lower risk of side effects. Keep in mind that a drug which is useful during the early stages of the disease may stop being effective as the brain changes.
Some patients may refuse to take their meds because they find it difficult to swallow the pill (in which case, physical therapy for dementia can help) or because the medication tastes bad. Gently remind them why they’re taking that pill and that it will help with symptoms. If they continue to refuse, ask their doctor if there are any alternatives, such as liquid medications, dissolvable tablets, or gummy bears. Sometimes compounding pharmacies can provide medications in these forms.
Non-pharmacological Treatments: Physical and Cognitive Therapy

Another way to help your loved one is to find a suitable type of therapy to promote their physical and cognitive well-being. Some patients are happy with therapy alone, while others benefit from a health care plan involving both medications and therapy combined.
Benefits of Physical Therapy
Physical activity is one of the best non-pharmaceutical ways to reduce or delay progression of symptoms, maximize function, and maintain quality of life. If you’re looking for a physical therapist, make sure they specialize in neurodegenerative disorders.
Physical therapy has many benefits for dementia patients. It can…
- Improve balance and decrease risk of falling: Falling is a real danger for patients with dementia, especially when the disease starts affecting balance and posture. Physical therapy can help improve stability, strength, and coordination.
- Strengthen muscles: Dementia doesn’t affect just the brain. It can also affect muscles. Physical therapy uses stretching and strengthening to help patients move more comfortably and enjoy their daily activities.
- Improve cardiovascular health: It may not be like training for a marathon, but physical therapy for dementia patients increases the heart rate enough to improve cardiovascular health and general fitness.
- Improve emotional symptoms: Physical activity helps release endorphins in the brain, which improve feelings of happiness and tranquility.
- Improve cognitive abilities: Physical therapy stimulates blood flow to the brain and improves cognitive function. This allows patients to think more clearly, improves mood, and increases overall quality of life.
- Reduce social anxiety: Patients may avoid going out in public due to fear of falling or embarrassment. Physical therapy increases fitness and helps to alleviate those fears.
- Build stronger social interactions: Attending physical therapy — especially in group sessions — provides patients with the opportunity to exercise and socialize at the same time. This can improve patients’ confidence, self-esteem, and general outlook.
- Educate the family: For many patients, physical therapists also play an important role in teaching the family about dementia. These therapists can educate caregivers about home safety, ways to reduce the risk of falling, and techniques to communicate better with someone living with dementia.
Benefits of Cognitive Therapy (Also Called Memory Therapy)
At Neural Effects, we believe dementia patients benefit most from multidisciplinary therapies. We combine cognitive therapy, reminiscence therapy, and occupational therapy — all of which address different symptoms at different stages of the dementia journey. This type of therapy (which we generally refer to as cognitive therapy) is also known as memory therapy.
For example, during the early stages of dementia, treatment emphasis is more on maintaining cognitive function using a variety of cognitive games, such as word games and puzzles. As the disease progresses, patients may need therapy to help find new ways to deal with their symptoms.
Similar to physical therapy, patients can benefit from engaging in memory therapy in different ways:
- Improve cognitive function: Cognitive therapy relies on different exercises to address cognitive symptoms, such as memory loss, difficulty concentrating on a particular task, and brain fog. This approach has been increasingly used to treat symptoms in dementia patients with very positive results.
- Stimulate social interactions: Any form of therapy can help dementia patients improve social interactions. For example, sharing memories from the past with a group and a therapist can be an enjoyable way to connect with a patient with dementia.
- Decrease stress: Therapy can also be seen as a tool to reduce stress. Reminiscence therapy, for example, can trigger pleasant feelings, boost mood, reduce agitation, and minimize challenging behaviors like wandering, anger, and more. This form of therapy can boost confidence in older patients with dementia because it’s something they’re still able to do.
- Stay independent: The role of a therapist is to work with patients to find ways to maintain their independence in their day-to-day activities. Therapy providers can assess the patient’s daily routine to identify which activities they wish to maintain or work towards.
- Improve quality of life: Therapists can suggest different ways to improve quality of life, from brain games to stimulate cognitive function to technology to use at home to ensure the patient’s safety.
- Educate the family: As well as providing practical advice for the patient, therapists can also help you learn techniques for home care.
The Benefits of Other Types of Therapy

A popular type of therapy for dementia patients is music therapy. Activities involving music can be an effective way to communicate with a person who has dementia and to unlock memories and feelings. Even in severe cases, when other skills are already lost, patients can still enjoy familiar songs and tunes.
Specialists in music therapy have extensive training in using music with dementia patients and can address some complex behaviors, such as depression and aggression. This therapy can improve disruptive behaviors, reduce anxiety, and generally improve mental health and quality of life for dementia patients.
Patients may also benefit from behavioral therapy specifically developed for dementia. It’s common for these patients to wander away from home because they feel restless. This type of therapy encourages patients to find other ways to deal with their restlessness, such as physical activity, to reduce problematic behavior. This therapy doesn’t stop the development of behavioral problems, such as aggression or delusional thinking, but it’s a useful tool to reduce these symptoms.
One other example of therapy available for dementia patients is bright light therapy. This has shown some promise in helping patients deal with symptoms like poor sleep and anxiety. Patients just need to sit next to a therapy light box for a certain period to reset their internal clock and help them relax and sleep better.
Therapy at Neural Effects

While most dementia patients receive cognitive-related therapies and physical therapy separately, we integrate the two for a more effective approach. Studies have confirmed that engaging in supervised cardiovascular exercise before cognitive therapy can improve cognitive functions such as thinking, concentration, and executive function.
Treatment with Neural Effects starts with a full evaluation of the patient’s health. We assess cognitive skills such as memory, attention, executive function, and language. Once this assessment is complete, you and your family members can meet with our team to discuss the results and suggest the best way forward.
Further reading: Dementia evaluation at Neural Effects
During treatment, our therapists use a variety of therapies based on the problems identified during the assessment. We offer exercises targeting attention, memory, thinking skills, language, vision, and many more. All this is combined with sessions of aerobic exercise to boost the results.
You can accompany your loved one during therapy at our clinic. Our therapists will teach both of you the exercises and how to adjust their difficulty so that you can continue treatment at home.
When Therapy Can No Longer Help the Patient
Many patients eventually reach a point where medication and therapy are no longer helping. In fact, therapy could become a source of stress (and put the therapist in danger if the patient grows belligerent and confused).
If you’re caring for a loved one with dementia, talk to them and their doctor about what to do when this situation arises. Some patients wish to continue treatment as long as possible, while others prefer to stop it as soon as they can no longer function by themselves.
If you know their wishes regarding long-term care, care facilities, and end-of-life arrangements, it’s easier to stop treatment when doing so is in their best interest. Discussing plans for late-stage dementia ahead of time also helps to minimize arguments amongst family members, who may have differing opinions on what their loved one’s dementia care plan should include.
Ways You Can Help Dementia Patients at Home
There are many adjustments you can make at home to help your loved one with dementia:
Balanced Diet
Ensure the patient follows a healthy and balanced diet. One of the recommended diets is the MIND diet, which includes green leafy vegetables, berries, nuts, whole grains, fish, and poultry. It avoids red meat, dairy products, sugary foods, and fried food. Other options include the Mediterranean diet and the Dietary Approaches to Stop Hypertension (DASH) diet, which also encourage consumption of fruits and vegetables and limit highly processed foods.
Patients with dementia may also benefit from dietary supplements to improve cognitive function. This includes, for example, polyunsaturated fatty acids, a variety of vitamins and minerals, and natural products such as ginseng or curcumin. However, it’s not always easy to assess which products could be helpful. We’ve compiled a list of different products and assessed the results from clinical studies for each one. To find out more about these products, read our post on ways to treat dementia naturally.
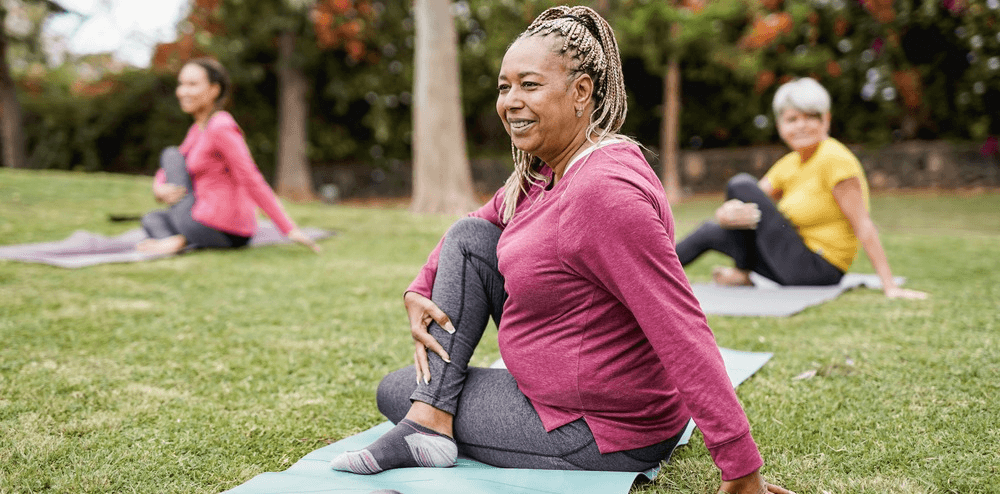
Regular Exercise
Encourage your loved one to engage in physical activities as part of their daily care. As described earlier, patients with dementia can benefit both physically and mentally from exercise.
We suggest about 30 minutes of exercise every day for at least five days a week. This doesn’t have to be all at the same time; you can break down these sessions into three sessions of 10 minutes each, for example. Local communities and sports centers often provide organized sessions of physical activity, including music and dance, swimming, or tai-chi. Walking, gardening, and housework are also good forms of everyday physical activity.
Good Sleep Patterns
Problems falling asleep or waking up frequently during the night are common in dementia patients. The best way to help these patients is to establish a healthy bedtime routine. It’s helpful to…
- Follow the same sleep schedule every day, including weekends and holidays.
- Set a relaxing mood in the evening.
- Avoid mobile phone or TV use in the bedroom before going to sleep.
- Restrict daytime naps to 20 – 30 minutes.
- Avoid caffeinated drinks in the afternoon and evening.
- Check medication. One side effect of cholinesterase inhibitors, for example, is insomnia. Taking the medication earlier in the day often helps, but check with the patient’s doctor before making any changes.
- Try melatonin. This supplement doesn’t improve cognitive function, but it often helps patients get a better night’s sleep. We recommend starting with a low dose (such as 0.5 mg) about 30 minutes before bed, then increasing the dose if needed. Consult with the patient’s doctor before starting any new supplement.
Keep the Brain Active
Another way to improve brain function is to keep the brain active. Instigate brain games, such as memory games, crosswords, puzzles, and so forth. These activities can improve memory and thinking, as well as reduce anxiety and stress. We suggest including at least 30 minutes of brain activities in their daily plan.
Maintain Regular Social Interactions
Maintaining regular social contact with friends and family can improve the lives of those with dementia. Studies suggest that even just one hour every week can significantly improve quality of life and reduce agitation levels. This includes, for example, joining an arts and crafts group, taking dance lessons, or simply getting together with friends to reminisce about the past. If they live in a nursing home, encourage them to participate in group activities. If they receive care at home, make sure they have access to transportation if needed.
Use Technology
Recent technological innovations can also help keep those diagnosed with dementia more comfortable and safe. This “assistive technology” can help patients stay independent for longer and manage risks at home.
Examples include adapted mobile phones with pre-programmed frequently dialed numbers and large displays, monitors that can alert caregivers if a device has not been switched off after use, and automated pill dispensers that beep when it’s time to take medication.
Join a Support Group
The Alzheimer’s Association has a 24/7 helpline, information on support services, and ways to find a support group and other local resources if you’re in the U.S. If you’re in the U.K., you can find caregiver support resources via the Alzheimer’s Society.
Being a dementia caregiver involves a rollercoaster of emotions and requires you to give much of yourself. When you take care of yourself and surround yourself with people who can encourage you and give you more resources, you’ll be able to provide a better quality of life for your loved one suffering from dementia.
Neural Effects uses the latest evidence-based techniques to diagnose and help dementia patients. We are located in Provo, Utah, and serve anyone in Salt Lake City or the Utah Valley area. We are in network for most types of medical insurance. Schedule your evaluation today.
