At the moment, there is no cure for dementia. However, there are multiple treatment options that can slow down cognitive decline from dementia and help patients stay independent for longer.
In most cases, patients are offered specific treatments to address specific symptoms. This can be, for example, physical therapy to improve fitness or medication to help with memory.
At Neural Effects, we believe one of the best options for dementia patients is a combination of exercise and cognitive stimulation therapy (CST) designed to slow cognitive decline and promote physical wellbeing. These therapy modalities are appropriate for most types of dementia, such as frontotemporal dementia, Alzhiemer’s disease, and Lewy body dementia. This approach can be used concurrently with other treatments for dementia, such as medications and supplements.
In this article, we explain the following dementia treatment options:
- Dementia treatment at Neural Effects
- Other non-pharmacological treatment options
- Pharmacological treatment options
- Dietary Supplements
- Lifestyle changes
Neural Effects uses the latest evidence-based techniques to diagnose and help dementia patients. We are located in Provo, Utah and serve anyone in Salt Lake City or the Utah Valley area. We are in network for most types of medical insurance. Schedule your evaluation today.
Dementia Treatment at Neural Effects

At Neural Effects, we use a combination of exercise and cognitive stimulation therapy (CST) to treat dementia patients. To our knowledge, we are the only U.S. clinic to offer this combination. We designed our treatment this way because research shows that patients benefit more from completing CST immediately after physical exercise than when just using CST on its own.
This increased benefit is thanks to a phenomenon in the brain called the post-exercise cognitive boost (PECB). PECB triggers the release of an important chemical called brain-derived neurotrophic factor (BDNF), which in turn makes the brain more receptive to change and promotes learning and memory.
BDNF levels naturally decrease as we get older, but dementia patients have extremely low levels. Boosting BDNF with exercise can improve cognitive function, mood, and behavior, as well as promote fitness and reduce the risk of falls.
Initial Visit and Diagnosis
All patients at our clinic, whether or not they have an existing dementia diagnosis, complete a neuropsychological exam (also called a neurocognitive evaluation) to find out how dementia has affected their cognitive skills. Our therapists conduct tests to assess memory, attention, and other cognitive skills. Patients also undergo exams to assess reflexes, eye movements, and balance. Finally, our therapists look for signs of anxiety, depression, or stress. This examination usually lasts around 2 to 2.5 hours.
Cognitive Care Plan
Once this evaluation is done, our team combines all the information to write a cognitive care plan (CCP). All patients who are assessed at Neural Effects receive a CCP, even patients whose evaluation does not reveal dementia. (The report still includes valuable information that will help these patients protect their cognitive health and understand their risk of dementia developing.)
The CCP includes:
- Brief summary of patient’s medical history
- Diagnosis
- Results from the assessment
- Risk factors and how the disease is likely to progress
- Lifestyle changes that may help the patient
- Ways the family can get involved
- Recommended treatment options at Neural Effects
Aerobic Exercise and Cognitive Stimulation Therapy
Patients attend 14 sessions of structured, one-hour-long group therapy sessions. Sessions run twice a week over seven weeks, each covering a different theme.
Sessions start with 10-15 minutes of aerobic exercise, typically done on a stationary bike. Our therapists understand that some patients have mobility issues, so these sessions are tailored to what the patients can do in a safe and controlled manner.
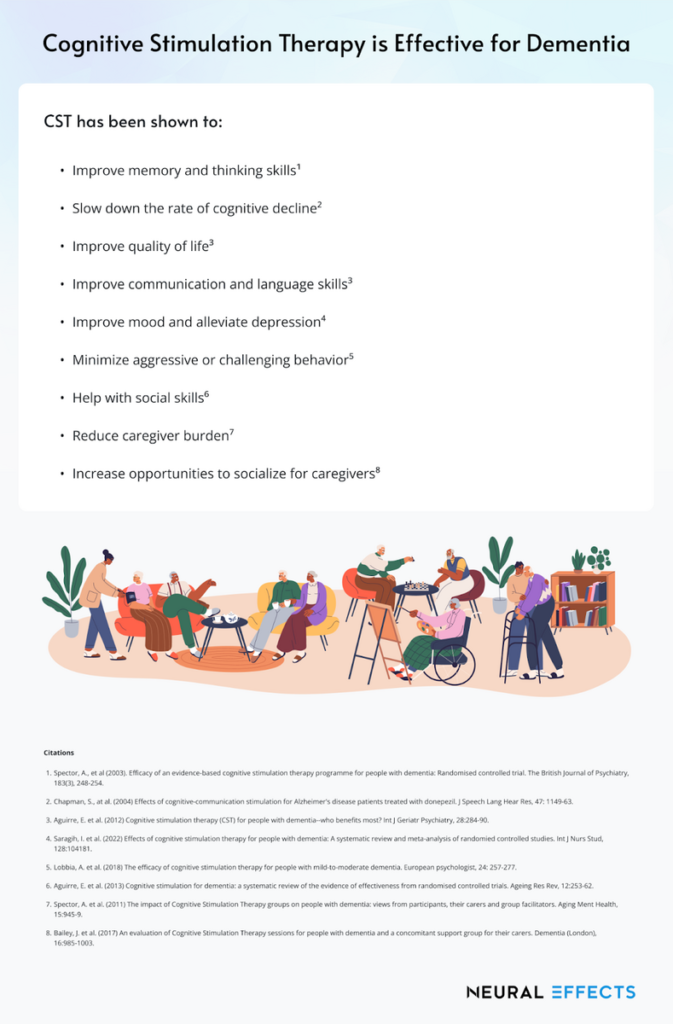
After exercise, patients have their CST sessions. This involves group activities designed to improve memory, problem-solving skills, and language abilities. Patients may engage in group discussions about current affairs, do puzzles or crosswords, listen to music, or do arts and crafts projects. Multiple clinical trials show that CST helps with cognitive skills such as memory, focus, and language. Overall, this therapy also boosts patients’ confidence and improves their quality of life.
We’ve written in more detail about the benefits of CST here.
If our therapists feel that patients may benefit from additional therapy, we refer them as needed to the appropriate specialists — such as neurologists, physical therapists, or psychologists.
Family Involvement
Family support is also an important part of our program. Family members and caretakers can attend the first session to learn about CST. This way, they can help patients by repeating some of the activities and games at home.
Our therapists also give resources to the family, suggest support groups, and educate caregivers about lifestyle changes that can help their loved ones.
Schedule your evaluation at Neural Effects today.
Other Non-pharmacological Treatment Options

Cognitive decline can be treated with a variety of non-pharmacological options that address psychological, behavioral, and physical issues.
Some of these options are general and can be adapted as the illness progresses, while others are more suited to specific stages of the condition. Some are more focused on addressing specific symptoms of dementia, while others may help slow cognitive decline.
Physical Therapy (Physiotherapy)
Physical therapists work with dementia patients and their carers to encourage physical activity and help them maintain their independence for as long as possible. Multiple studies show physical therapy can have positive effects on cognitive and physical skills in patients with MCI and dementia, including lower risk of falls, increased fitness, better sleep, and improved mood.
Further reading:
Occupational Therapy
Occupational therapy is ideal to help dementia patients stay independent for as long as possible. Occupational therapists can suggest exercises to make daily activities (such as getting dressed or eating) easier for older adults, help to establish a routine to provide structure and stability, and recommend equipment such as mobility aids or support bars for the bathrooms.
Further reading: Occupational therapy for dementia patients
Speech and Language Therapy
Speech and language therapists can help dementia patients with communication and language issues, such as difficulty with attention and focus, voice and speech problems, and difficulty reading. These therapists also assess and treat swallowing problems, which are common as the disease progresses.
Reminiscence Therapy
During therapy, patients are invited to reminisce about events and experiences from their past. Therapists often use props, such as videos, music, pictures, and objects that hold a particular meaning for the patient.
Possible topics include:
- Childhood events
- Favorite playground games/board games
- Food likes and dislikes
- Pets and animals
- Family and relationships
- Music
- Favorite sports teams
Talk Therapy
The main aim of talk therapy is for patients to discuss their feelings and worries, including how they feel about their disease. Some patients find it easier to discuss their problems with a therapist rather than with their family members. Talk therapy can reduce symptoms of depression and anxiety and is a good avenue for patients to work on their mental health.
Art Therapy
Many dementia patients enjoy creative activities, such as sculpting, painting, drawing, making cards, creating jewelry, or participating in community art projects. This therapy reduces agitation and gives patients a sense of purpose by providing an opportunity for nonverbal expression. Art therapy can improve cognitive function, enhance communication, and promote social interaction for dementia patients.
Music Therapy

Music therapy can be used with dementia patients during all stages of the condition. It improves behavior problems, lowers anxiety, and controls agitation. During the early stages, patients can be more active and play a musical instrument, sing, or attend musical concerts. In the later stages, patients can still enjoy listening to familiar songs that may help unlock memories from the past. With the right adjustments, music therapy is appropriate for long-term care.
Pet Therapy (Animal-Assisted Therapy)
Petting a cat or a dog can reduce agitation and aggression as well as improve the patient’s mood. It can also promote social interactions if done as a group and stimulate physical activity for patients who can still go out and play with an animal.
Reality Orientation Training
Reality orientation training involves repeating basic information, such as the patients’ name, where they live, and the date. The therapist may use clocks and calendars on the wall or signs and labels on doors, cupboards, and other objects. This approach can improve orientation, but most changes are short-lived.
Validation Therapy
This therapy is the opposite of reality orientation training. The therapist makes no effort to remind patients about the date or where they live but instead engages with patients within their reality. Some studies found that it helps with agitation and supports caregivers, while others found no significant benefits.
Sensory Stimulation Therapy (Sensory Integration Therapy)
Sensory stimulation therapy is designed to help patients remember positive emotions and memories. The aim is to use the five senses — hearing, sight, smell, taste, or touch — to trigger happy memories and make patients feel safe and relaxed. It could involve triggers such as a familiar meal or a bouquet of their favorite flowers.
Massage and Aromatherapy

Massage and aromatherapy can be calming for dementia patients. Therapists can use different essential oils, such as lavender, chamomile, and lemongrass, for example, to promote relaxation. Not all patients enjoy this therapy because they either don’t like being touched or find the smells too strong. It should also be avoided in patients with skin conditions such as psoriasis or eczema.
Doll Therapy
Dolls therapy is particularly useful for late-stage patients. Some patients enjoy holding a doll (or a teddy bear) and reminiscing about events from their childhood. Playing with dolls improves the patient’s mood, promotes social interaction, and reduces the incidence of delirium episodes. Doll therapy also reduces the use of antipsychotic drugs, prevents wandering, and improves the quality of life.
Bright Light Therapy
Bright light therapy can be beneficial in treating sleep disturbances in dementia patients. It improves the patient’s mood and reduces symptoms of anxiety and depression. During a session of bright light therapy, patients sit in front of a light that provides about 30 times more light than the average light for a set amount of time. This resets the patient’s internal clock, which is often disrupted from dementia.
Pharmacological Treatment Options

There are also several different pharmacological options to treat dementia patients. These can be used in combination with the non-pharmacological options described above. The main types of medication that can be used include:
- Aducanumab
- Cholinesterase Inhibitors
- Glutamate regulators
- Antipsychotics
- Antidepressants
- Sedative hypnotics (sleeping pills)
Some of these prescription drugs help slow down the patient’s cognitive decline, while others are used to address specific symptoms. We always recommend that patients be reassessed regularly by their doctor once they start medication. It’s also important to ensure that caregivers understand the patient’s medication and potential side-effects, allowing them to make informed decisions concerning their loved one’s health.
Aducanumab
In 2021, the FDA approved a new therapeutic drug called Aducanumab (Brand name: Aduhelm) designed for treatment of Alzheimer’s disease.
How does Aducanumab work?
Aducanumab targets beta-amyloid, a protein that accumulates in the brain of dementia patients and forms plaques. These plaques block communication between neurons and trigger an immune response against the body’s own nerve cells. Participants in one clinical trial experienced a small improvement in memory and thinking skills but did not report any significant improvements in day-to-day life.
Important considerations:
- There is some controversy surrounding its FDA approval as there is no definitive evidence that removing the plaques produces symptom improvement, and side effects are dangerous; further research is needed.
- This drug has not been approved in Europe yet.
- It has only been tested in patients with mild cognitive impairment (MCI) and early-stage dementia.
- Potential side effects are serious and include brain swelling, small brain bleeds, headaches, increased risk of falls, diarrhea, and confusion.
Cholinesterase Inhibitors
Cholinesterase inhibitors are the most common prescription drugs used to treat dementia patients, including patients with Parkinson’s disease. At the moment, there are three types:
- Donepezil (Brand name: Aricept)
- Galantamine (Brand name: Galantyl, Razadyne)
- Rivastigmine (Brand name: Exelon)
How do cholinesterase inhibitors work?
Acetylcholine helps nerve cells in the brain communicate with each other. Cholinesterase inhibitors block an enzyme called acetylcholinesterase from breaking down acetylcholine. This increases levels of acetylcholine and improves brain function. Patients can experience improvements in memory, thinking, language, judgment, and decision-making.
Important considerations:
- Cholinesterase inhibitors are prescribed for patients with mild-to-moderate Alzheimer’s disease.
- These drugs are usually well-tolerated, but some patients experience nausea, vomiting, loss of appetite, and increased frequency of bowel movements. Side effects typically resolve over time.
- Side effects can be minimized by increasing the dose gradually and ensuring patients always eat something when they take their medication.
- There are no significant differences in effectiveness between the three options; however, patients who do not respond to one type may respond better to another.
- Cholinesterase inhibitors are safe for most patients, but those with a history of peptic ulcers or heart conditions should be monitored closely.
Glutamate Regulators
Memantine is the only glutamate regulator used to treat patients with moderate to severe cases of Alzheimer’s Disease. It can be prescribed by itself (Brand name: Namenda) or combined with a cholinesterase inhibitor (Brand name: Namzaric).
How do glutamate regulators work?
As nerve cells start to die in the brains of dementia patients, they release glutamate, which causes problems for the patients. Glutamate regulators protect the remaining nerve cells by blocking the effects of excessive glutamate. Patients experience improved memory, attention, reasoning, and language.
Important considerations:
- Memantine is usually well-tolerated, although the dose may need to be reduced in patients with renal conditions.
- Possible side effects include headaches, nausea, vomiting, loss of appetite, constipation, increased frequency of bowel movements, confusion, and dizziness.
- Memantine is prescribed to patients with moderately severe Alzheimer’s Disease.
- There’s some evidence that these meds can help patients with Lewy bodies dementia, vascular dementia, and mixed dementia.
Antipsychotics
Some patients in the later stages of dementia develop emotional and psychological symptoms such as agitation, aggression, and hallucinations. These symptoms can be very stressful, both for the patient and their caregivers. In some circumstances, antipsychotics may be helpful to address these symptoms.
How do antipsychotics work?
For extreme or persistent cases, doctors may prescribe antipsychotic drugs such as risperidone or haloperidol. Dopamine is a chemical present in the brain that is involved with thinking, emotions, and behavior. However, too much dopamine can cause behavioral issues. In simple terms, antipsychotics block the effects of dopamine and reduce the symptoms.
Important considerations:
- Antipsychotics should only be used as a last resort.
- These drugs should be used at the lowest possible dose and only for short periods to avoid serious side effects.
- Ultimately, the decision to start and stop antipsychotics should be made by a psychiatrist or other healthcare professional with experience in treating patients with neurological conditions.
- Antipsychotic drugs can cause serious side effects, including drowsiness or confusion, shaking, risk of falls and fractures, stroke, and infections.
Antidepressants
It’s common for dementia patients to develop anxiety and depression. If patients don’t respond well to non-pharmacological options (which should be tried first), antidepressants may help improve mood, control irritability, and reduce anxiety.
How do antidepressants work?
The most common antidepressant drugs used in dementia patients are called selective serotonin reuptake inhibitors (SSRIs). SSRIs work by increasing serotonin levels in the brain. After carrying a message between nerve cells, serotonin is reabsorbed. (This is known as “reuptake.”) SSRIs block this mechanism, which means more serotonin is available to improve communication between nerve cells.
Important considerations:
- It may take weeks or months for patients to feel any benefits; consistency in taking the medication is key to success.
- SSRIs are usually well-tolerated by patients with dementia, but some may experience headaches and nausea, especially during the first two weeks of treatment.
- There is some controversy surrounding the use of SSRIs for dementia patients. Patients and their family caregivers should discuss the benefits and risks carefully with their medical providers before starting their use.
Sedative Hypnotics (Sleeping Pills)
Struggling to fall asleep or waking up during the night can cause many difficulties for dementia patients and lower quality of life. In addition, some drugs used to treat other symptoms can cause patients to feel drowsy during the day but not sleepy at night.
How do sedatives hypnotics work?
In general, sedative-hypnotics target different receptors in the brain to “slow down” the nervous system. Some meds are designed to induce sleep, while others are used to help patients stay asleep.
Important considerations:
- Sleep medication for dementia patients should be used as a last resort, but it can be useful for some patients.
- These drugs can be prescribed for occasional use when the patient feels they need a good night’s sleep. Taking these every night may lead the patient to become completely reliant on medication to sleep.
- Long-term, consistent use of sleep medications can be dangerous for dementia patients. They lead to an increased risk of falls and fractures, confusion, and a decline in the ability to care for oneself.
- It’s important to discontinue their use after a regular sleep pattern has been established.
Neural Effects uses the latest evidence-based techniques to diagnose and help dementia patients. We are located in Provo, Utah and serve anyone in Salt Lake City or the Utah Valley area. We are in network for most types of medical insurance. Schedule your evaluation today.
Natural Treatment Options (Dietary Supplements)

There are many different dietary supplements promoted as memory enhancers or treatments to delay the progression of dementia. However, the Food and Drug Administration (FDA) doesn’t require the same rigorous approval process for supplements as it does for a new prescription drug. This makes it difficult for patients to determine which dietary supplements are worth taking (if any) to reduce dementia symptoms.
In this article, we’ve listed the most commonly recommended products, along with study results, in the following sections. This is just for your information, and we always recommend that you consult with your healthcare provider before starting on any supplements.
Polyunsaturated Fatty Acids
Docosahexaenoic acid (DHA) is a long-chain omega-3 polyunsaturated fatty acid involved in multiple mechanisms in the brain. People who eat fish on a regular basis (an important source of DHA) experience a slower rate of cognitive decline and are less likely to have memory loss.
Good sources of DHA include dark meat fish such as tuna, salmon, and mackerel. DHA supplements are also available, typically made from fish oil or algae.
Vitamin D3
Vitamin D — from food or via our skin when stimulated by sunlight — is vital for normal brain function. A few studies suggest vitamin D3 supplementation may improve some aspects of cognitive function, but further research is needed.
Supplementation is safe at low levels, but excessive amounts may cause nausea, vomiting, confusion, and heart rhythm abnormalities. It’s important to check with your doctor before starting to take vitamin D3 supplements, especially in patients with overactive kidney and liver disease, diabetes, and hypotension.
Vitamins B6, B9, and B12
Vitamins of the B complex — B6 (pyridoxine), B9 (folic acid), and B12 (cobalamin) — are involved in many mechanisms in the body. Studies seem to suggest that vitamin B supplementation can help patients with mild cognitive impairment improve verbal fluency, processing speed, attention, and working memory.
Vitamin B supplements are safe for most people when taken at recommended doses but may interact with some prescription drugs.
Vitamin E
Vitamin E works as an antioxidant and protects cells from oxidative stress. The brain is highly susceptible to oxidative stress, which contributes to cognitive decline. Some studies showed that vitamin E supplementation can help patients with mild forms of dementia experience a slower cognitive decline, but further research is needed.
Good sources of vitamin E include green leafy vegetables, sunflower seeds, and almonds. Vitamin E is also available as pills or chewable tablets.
Ginseng
Commonly used in Chinese medicine, the roots of ginseng contain a compound called ginsenoside, which has antioxidant and anti-inflammatory properties. Studies suggest that ginseng can slow down the progression of symptoms, but any improvements disappear when patients stop taking the supplements.
Panax ginseng is safe for most patients, but it may cause insomnia, rapid heartbeat, and high blood pressure in high doses or when combined with certain prescription medications.
Coconut Oil and Medium-Chain Triglycerides
Medium-chain triglycerides are a naturally occurring type of fat present in coconut oil. These fats are easily used by the brain as an energy source. Studies show that supplementation may help dementia patients, but these benefits are short-lived and disappear once supplementation stops. These supplements are generally considered safe, but gastrointestinal side effects are common.
Huperzine A
Huperzine A — derived from several species of firmoss plants — can increase the levels of neurotransmitters and help brain function. Clinical trials reported improvements in cognitive function, but because huperzine A works in a similar manner to some Alzheimer’s drugs, it is unlikely to help patients who are already taking these drugs.
Huperzine A is available as a dietary supplement. It seems safe for short-term use, but no evidence supports long-term use.
Curcumin
Used in Asian medicine, curcumin is one of the most important components of turmeric. People who eat food with curcumin (curries and other Indian dishes, for example) seem to have improved cognitive function, but a study using curcumin supplements failed to show any benefit.
The main source of curcumin is turmeric, but curcumin supplements are also available.
Coenzyme Q10
Coenzyme Q10 (CoQ10) is an antioxidant naturally produced by the body. In theory, it should help dementia patients, but clinical trials with patients with Alzheimer’s disease failed to show any cognitive benefits after four months of supplementation.
CoQ10 can be found in certain foods like oily fish, whole grains, and fruit. CoQ10 supplements are available over the counter.
Ginkgo Biloba
Used in combination with conventional medication, Ginkgo biloba can help cognitive performance as well as behavioral and psychological symptoms caused by dementia. However, results are inconsistent and unreliable.
Ginkgo biloba is safe for most patients, but it’s not advised for patients with high blood pressure.
Resveratrol
Resveratrol may help dementia patients improve their ability to complete daily tasks, but studies detected no effect on cognition or executive function. Good sources include red wine, grapes, berries, chocolate, and peanuts. Short-term supplementation is considered safe for most patients, but long-term use has not been studied.
Zinc with Vitamin C
Zinc and vitamin C are involved in how nerve cells communicate with each other. A combination of zinc and vitamin C can improve attention and may help slow down cognitive decline. There are supplements available with this combination.
Lifestyle Changes

In addition to pharmacological and non-pharmacological interventions, dementia patients also have the option to make important lifestyle changes that can help slow down the progression of symptoms and improve their quality of life. These changes are especially effective if lifestyle choices were an underlying cause of their dementia.
Eat a Balanced Diet
For patients with dementia, a healthy and balanced diet is one of the best ways to slow down the progression of the disease. One example of a healthy diet for the brain is the MIND diet, which includes green leafy vegetables, berries, nuts, whole grains, fish, and poultry and avoids red meat, dairy products, sweets, and fried food. Following this diet is associated with a slower decline in cognition, equivalent to being 7.5 years younger.
Patients can also follow the Mediterranean diet and the Dietary Approaches to Stop Hypertension (DASH) diet, as both encourage the consumption of fruits and vegetables and the avoidance of sugary treats and processed food. At our clinic, we primarily teach the Mediterranean diet.
Engage in Regular Exercise
Physical activity can help dementia patients both physically and mentally. Any kind of exercise can help, including participating in organized sports or activities like walking, dancing, or gardening. Ideally, patients should engage in 30 minutes of exercise per day, five to seven days per week. Benefits of regular physical activity include:
- Better cardiovascular health and fitness
- Improved ability to perform activities of daily living (ADLs) such as getting dressed, cleaning the home, and cooking meals
- Slowed cognitive decline
- Better sleep
- Increased opportunities for social interaction
- Lower risk of falls
- Improved mood and self-esteem
Follow a Healthy Sleep Routine
It’s common for dementia patients to experience sleep disturbances, such as difficulty falling asleep at night or drowsiness during the day. Some dementia patients also experience “sundowning,” where they feel confused, agitated, and aggressive in the evening. To promote better sleep:
- Check for medical conditions, such as depression or sleep apnea, which can disrupt sleep.
- Check medication side effects. Some medications — including donepezil, for example — can cause insomnia. It may be better to take these earlier in the day; check with a doctor before making any changes.
- Follow the same routine every day by going to bed and getting up at the same time. This includes weekends and holidays.
- Avoid alcohol and caffeinated drinks, especially at night.
- Avoid the use of screens before going to bed.
- Engage in some physical activity during the day to promote better sleep at night.
- Limit daytime naps to 20-30 minutes.
- Create a peaceful and relaxing mood before going to bed. End the day with a relaxing activity such as listening to calming music or reading a book.
- Consider taking melatonin. Melatonin can help improve sleep and reduce sundowning in people with dementia. Start with a low dose (under 5 mg) about 30 minutes before bed, then gradually increase the dose if needed.
Challenge the Brain
One way to slow down cognitive decline is by keeping the brain active. For example, cognitive training with “brain games” can help with certain aspects of memory and thinking and reduce anxiety and stress. Examples of cognitive activities include:
- Playing games and puzzles
- Learning a new skill, such as how to play a musical instrument
- Reading
- Using apps for brain games
- Rekindling an old hobby or finding a new one
- Engaging in activities that require coordination, such as arts and crafts
Patients should engage in brain activities for at least 30 minutes every day. It’s important to choose something the patient enjoys doing and can still complete without getting frustrated.
Engage in Regular Social Activities
Losing contact with friends and family accelerates the progression of the disease and increases the risk of developing anxiety and depression in dementia patients. To avoid this, patients should engage in regular social activities, such as going out with friends, joining a new group, or taking dance lessons. Social interaction can be helpful even for patients who are in the later stages of the disease and have difficulty communicating. Some nursing homes and other care facilities organize regular activities that encourage their residents to socialize regularly. Patients can also look for support groups in their area, both for the patient and for caregivers.
Neural Effects uses the latest evidence-based techniques to diagnose and help dementia patients. We are located in Provo, Utah and serve anyone in Salt Lake City or the Utah Valley area. We are in network for most types of medical insurance. Schedule your evaluation today.
