Cognitive therapy — also known as memory therapy — includes interventions that are designed to directly or indirectly protect cognitive skills. Evidence shows that patients with mild cognitive impairment (MCI) or most types of dementia (Alzheimer’s disease, vascular dementia, etc.) who regularly engage in cognitive therapy perform better in thinking, reasoning, attention, memory, and other cognitive skills.
Types of cognitive therapy include:
- Cognitive stimulation therapy (CST)
- Cognitive rehabilitation therapy
- Cognitive training therapy
- Reminiscence therapy
- Reality orientation therapy
- Cognitive behavioral therapy
In general terms, these non-pharmacological interventions involve some kind of brain-challenging activities. Although the overall aim of each differs (as we’ll see later), these therapies overlap significantly in the exercises and tools used. In fact, many therapists and other healthcare providers blend exercises from the different therapy modalities to best suit the needs of the patient.
Based on the evidence (which we describe in detail below), we believe the most well-rounded type of cognitive therapy currently available for patients with dementia is cognitive stimulation therapy (CST). This is the therapy we use with our patients.
This article will describe the different types of cognitive therapy, delve into how they can help patients with dementia, and give some example activities from them (where possible).
Neural Effects uses the latest evidence-based techniques to diagnose and help patients with dementia. We are located in Provo, Utah and serve anyone in the Salt Lake City or Utah County area. We are in network for most types of medical insurance. Schedule your evaluation today.
Cognitive Stimulation Therapy

During cognitive stimulation therapy, patients are exposed to a wide range of different brain-boosting activities. The aim is to slow down cognitive decline from dementia rather than targeting one specific cognitive function. CST is most effective in a group setting, but it can also be delivered to individual patients. This type of therapy can help older adults with mild to moderate dementia, but it’s not suitable for patients in the later stages of the disease.
In practical terms, CST includes 14 one-hour sessions run twice weekly for seven weeks. Each session includes a discussion about different subjects, such as current affairs, food, or movies. Patients also engage in cognitive games, such as puzzles and word games, and in creative activities, such as arts and crafts or baking. Every session is carefully designed to stimulate executive function and language skills, to help the individual continually develop new ideas and associations, and to encourage learning.
Types of Cognitive Stimulation Therapy
CST was originally developed to be used in a group setting, typically involving 6–8 patients and two facilitators. CST has been adapted for other situations, including:
- Maintenance CST (mCST)
- Virtual CST (vCST)
- Individual CST (iCST)
Maintenance CST is offered as a continuation of CST. Usually, this involves 24 further sessions done weekly in a similar way to standard group CST. Sessions may include discussions, cognitive games, creative activities, and mild exercise. Studies show this therapy can improve thinking abilities, general well-being, and quality of life for patients.
Virtual CST sessions appeared during the COVID-19 pandemic when patients were not allowed to socialize in person. Activities used are similar to standard CST but adapted to digital form. For example, the facilitator might share online news clips for the group to discuss. This type of therapy can slow down dementia progression and help patients feel less isolated. However, low levels of digital literacy may prevent widespread use with elderly patients, and it may not suit everyone, especially patients who suffer from hearing or visual impairments.
Individual CST sessions can be carried out at home. They’re often administered by the caregiver or a family member who receives some training on how to lead sessions. These sessions improve the relationship between caregiver and patient and help with quality of life, but are not as beneficial as starting with group therapy. It is especially helpful to encourage ongoing CST at home after the patient has received group CST and maintenance CST.
Is CST Effective for Patients with Dementia?
Multiple studies and clinical trials show that cognitive stimulation therapy can protect cognitive function in dementia patients as well as improve their mental health and quality of life. Patients report improvements in memory and thinking, which leads to increased self-esteem and more confidence to engage in social interactions. Indirectly, it also helps caregivers and their relationship with the patient.
Overall, cognitive stimulation therapy can:
- Help with short-term memory and thinking skills
- Slow down the rate of cognitive decline
- Improve quality of life
- Improve language skills and willingness to participate in conversations
- Improve mood and alleviate mental health conditions such as anxiety and depression
- Help with social skills
- Reduce aggressive or challenging behavior
- Help some patients prevent cognitive impairment more when combined with prescription drugs
- Help caregivers manage patients
- Increase opportunities to socialize for caregivers and loved ones
Further reading: Find cognitive stimulation therapy near you
Treatment at Neural Effects

At Neural Effects, our treatment program combines CST with short bursts of physical activity. Research shows that patients benefit more from cognitive therapy when it’s done after exercise rather than on its own. Exercise triggers the release of an important brain chemical called brain-derived neurotrophic factor (BDNF), which makes the brain more receptive to change and supports learning and memory.
Before treatment starts, patients complete a neuropsychological exam (also called neurocognitive assessment) to find out how dementia has affected their cognitive skills. In addition to reviewing the patient’s medical history, our team conducts tests to evaluate cognitive, physical, and emotional symptoms. This examination usually lasts around 2–2.5 hours.
After this exam, our team creates a cognitive care plan (CCP). Even patients who decide not to continue treatment with us receive this plan. It contains valuable information for all patients about their assessment, recommended lifestyle changes, and resources for the family.
The CCP includes:
- Results from the assessment
- Risk factors and how the disease is likely to progress
- Lifestyle changes that may help the patient
- Ways the family can get involved
- Recommended treatment options at Neural Effects
Every therapy session starts with 10–15 minutes of aerobic exercise, usually done on a stationary bike. Some of our patients have mobility issues, but exercises are tailored to what patients can do in a safe and controlled manner. This is followed by the CST part of the session, involving group activities designed to improve memory, problem-solving skills, and language abilities.
If our therapists feel that the patient may benefit from further therapy or other treatment types, we can refer them to the appropriate specialists and clinicians (from occupational therapy to geriatric psychiatry, to name just a few).
Neural Effects uses the latest evidence-based techniques to diagnose and help patients with dementia. We are located in Provo, Utah and serve anyone in the Salt Lake City or Utah County area. We are in network for most types of medical insurance. Schedule your evaluation today.
Cognitive Rehabilitation

Cognitive rehabilitation was originally developed to help patients with brain injuries, but doctors soon realized it could be equally applied to patients with neurodegenerative diseases such as dementia.
Cognitive rehabilitation refers to a customized approach to support patients with cognitive impairments. Patients have one-on-one sessions with a practitioner, usually at home. Patients, carers, and therapists work together to identify personally relevant goals and devise strategies for addressing them. The aim is not to promote cognitive skills in isolation, but to instead improve functioning and the ability to carry out daily tasks. These goals need to be specific, achievable, and realistic. If not, the patient will end up getting frustrated and stopping therapy.
For example, patients may want to relearn how to cook a hot meal because they have burnt things repeatedly in the past. In this case, therapy may consist of developing new ways of using kitchen appliances safely. They might also follow simplified recipes to shorten cooking time and use timers and other memory aids to remind them when food is cooked.
There are a number of rehabilitative strategies that patients with dementia can use to overcome their deficits and achieve their goals, such as:
- Mnemonics: This technique helps patients retain information. Patients can use visual imagery, poems, or acronyms to remember information.
- Chunking: Patients group similar information together to make it easier to remember. This could be organizing a shopping list based on the items’ locations in the supermarket, such as fruit and veggies, meat, cleaning products, etc.
- Method of loci: This is similar to using mnemonics but uses specific locations. For example, when patients need to memorize a list, they can picture themselves at home putting list items in different locations. When they need to recall the items, they can mentally go from room to room “looking” at the items.
- Recall: Therapists work with patients on ways to remember names, numbers, lists, and others. These exercises help with short-term and long-term memories.
- Prompting: Therapists start by giving plenty of prompts to complete a task, including verbal clues or gestures, but gradually offer less information. The aim is for patients to complete the task independently while prompting themselves.
- Chaining: This technique is useful for learning sequential tasks, such as waking up, brushing teeth, getting dressed, and making breakfast. Patients learn the sequence, and each step becomes a prompt for the next.
Is Cognitive Rehabilitation Effective for Dementia?
A systematic review of studies and controlled trials has shown that cognitive rehabilitation therapy can help dementia patients maintain their independence longer. Improvements are still noticeable up to 12 months after therapy. Patients report feeling more confident about completing daily tasks, including doing household chores, shopping, using appliances safely, and keeping track of important information.
Cognitive rehabilitation can help with memory, attention, and concentration, which in turn leads to a better quality of life.
In general terms, the benefits of cognitive rehabilitation include:
- Improved ability to carry out daily tasks
- Improved word recall
- Improved attention
- Slowed memory loss
- Improved quality of life for both patient and carer
- Decreased anxiety and depression
Cognitive Training

Cognitive training was originally developed in the 1970s to treat victims of stroke and head trauma. It proved very successful, and in the 1980s, doctors started using it with individuals suffering from dementia.
This type of therapy — also called brain training, retraining, or remediation — involves practicing a set of standardized tasks. These tasks are designed to improve specific cognitive skills, such as attention, memory, and problem-solving. They often involve activities and games that mimic activities of daily living. Ideally, tasks need to be tailored to the patient’s abilities and change as needed. Patients can access many programs online which work like video games, but there are pen and paper options which can be facilitated by family members or a therapist.
This therapy is based on the principle that practicing a specific task helps patients improve (or at least slows decline) in that particular cognitive skill. There is no evidence that patients will experience benefits in other cognitive skills. For example, memorizing lists helps with memory but not with problem-solving skills.
Recently, the definition of cognitive training has broadened to include strategy training, where patients practice strategies to cope with certain daily tasks — such as doing online shopping or setting up the table — using a variety of techniques including mnemonics and visual imagery.
Some examples of activities done during cognitive training include:
- Completing jigsaw puzzles: Puzzles help with visual-spatial skills. In turn, this helps patients organize visual information and interpret patterns.
- Playing music or singing: Playing a musical instrument helps brain function. Patients learn sequential information, which helps with memory and recall.
- Learning to dance (or other physical skills): Learning new dance steps helps with hand-eye coordination, as well as visual recognition and decision-making. It’s also good for fitness and social interactions.
- Playing cards: Playing card games helps boost memory, thinking, and decision-making. It can also promote social skills when games involve more than one person.
- Word, number, and picture puzzles: Games like crosswords, anagram games, Sudoku, word search puzzles, and ‘spot the difference’ images help with memory, word recall, and thinking.
- Engaging in conversation: A simple conversation can help with thinking, memory, language, and communication skills. Patients need to be able to follow and interpret what’s being said.
Is Cognitive Training Effective for Dementia Patients?
Studies show that cognitive training leads to improvements in multiple cognitive skills, including verbal fluency, learning, executive function, and processing speed, to name just a few. This therapy also helps improve mood and decrease depression. These benefits may be comparable (or even stronger in some cases) than what patients can gain from taking dementia medications like cholinesterase inhibitors, while avoiding the adverse effects associated with these medications. Crucially, it seems that patients can maintain these gains for a period after they stop therapy (between 3–12 months).
There is some evidence to support that cognitive training can produce these positive results because it changes patterns of neural activity in the brain of dementia patients. This means the brains of these patients remain highly plastic and capable of responding to cognitive therapy.
Cognitive training can:
- Improve memory and recall
- Improve verbal fluency and communication with others
- Improve processing speed and executive function
- Improve mood
- Reduce the incidence of depression symptoms
Reminiscence Therapy

Reminiscence therapy was introduced to dementia care as a standalone type of therapy in the late 1970s. Today, it can be done in isolation or in conjunction with other types of therapy, such as cognitive stimulation therapy, for example.
In simple terms, reminiscence therapy involves discussing events and experiences from the patient’s past to evoke memories, stimulate cognitive skills, and improve well‐being. Therapists often use props, such as videos, pictures, music, and objects that hold a special meaning for the patient. Care facilities can also use reminiscence to guide their design. For example, bedrooms in nursing homes can be made to resemble the patient’s own room at home to make it seem more familiar and help maintain the feeling of independence.
Possible reminiscence topics include:
- Childhood holidays
- Favorite playground games/board games
- Food likes and dislikes
- Pets and animals
- Family and relationships
- School days
- Favorite music
- Sports
- Cars
Types of Reminiscence Therapy
In general terms, reminiscence therapy can be divided into three categories:
- Simple reminiscence: This involves the recall and sharing of random memories and stories.
- Life review: This is a more structured approach, where patients cover their life story chronologically, looking at both positive and negative memories. Some patients like to create a “memory box” containing personal objects.
- Life review therapy: This option is aimed at patients battling symptoms of depression or other mental health problems. The aim is to look at past memories with a positive view of life. This is known as “life story work” and is becoming increasingly popular. Patients often produce a life story book portraying key elements of their lives.
Is Reminiscence Therapy Effective for Patients with Dementia?
Multiple studies show that reminiscence therapy can help with cognition while patients are attending sessions, but the effects can’t always be sustained once sessions are complete. This therapy reduces the incidence of depression symptoms and improves mood, especially in patients with mild to moderate dementia who are living in residential or nursing homes.
Reminiscence therapy can temporarily:
- Improve cognition
- Improve communication and language
- Improve quality of life of patients and carers
- Reduce the risk of depression and promote a positive attitude
- Improve relationships with others
- Improve social interactions
Reality Orientation Therapy

Reality orientation is another type of cognitive therapy. It was first described in 1966 as a rehabilitation method used for elderly patients, but it was used before that to help severely confused war veterans. In reality orientation therapy, the therapists present the patients with constant reminders about the date and time, where the patient is, and any other relevant information about the patient’s personal life or current events.
This type of therapy is better suited for patients in the middle stages of the disease. As the condition progresses, it gets harder for patients to remember these details, and it may be counterproductive to be constantly disagreeing with them. In recent years, this therapy has lost some of its popularity, and it’s used less frequently. However, a number of its ideas have been incorporated into other therapies like cognitive stimulation therapy.
Overall, the aim is to help the patient “stay” in the present and give them a greater understanding of their surroundings. This reduces confusion and disorientation and increases self-esteem.
Typically, reality orientation therapy involves:
- Talking frequently about objective realities, such as the day, time of day, date, and season
- Using important names frequently
- Discussing current events
- Referring to clocks and calendars
- Placing signs and labels on doors, cupboards, and other objects
- Asking questions about photos or other memorabilia
Types of Reality Orientation Therapy
There are two main types of reality orientation therapy:
- 24-hour immersive therapy
- Classroom therapy
Immersive therapy can be done with patients who live in a dedicated living facility full-time. At every interaction, health care workers and therapists reinforce date, time, location, and any special events with the resident. Caregivers often read the newspaper or watch the news with the patient to reinforce reality. In addition, clocks and calendars in the facility are constant reminders for the patients.
Classroom therapy is less intensive. Patients attend group sessions where therapists lead them in orientation-related activities. They also have a board with important information, such as date, time, weather, and current details. Therapists often encourage the patients to socialize, which also protects cognitive function.
Is Reality Orientation Therapy Effective for Dementia Patients?
Many studies show that reality orientation can help cognitive function in dementia patients, especially if combined with medication. After therapy, patients experience improvements in word recall, memory, sleep quality, and attention while showing fewer signs of depression.
Overall, reality orientation therapy helps patients by:
- Improving cognitive skills
- Improving communication skills, such as word recall and naming objects
- Improving memory and attention
- Improving quality of life for the patient and the caregiver
- Improving ADLs
- Reducing signs of depression
- Improving sleep
- Delaying the need to go into a nursing home
Comparing Cognitive Therapy Types
In the following chart, we summarize the five therapies covered in this post so far:
| Types of Cognitive Therapy for Dementia | |||||
| Cognitive stimulation | Cognitive training | Cognitive rehabilitation | Reminiscence | Reality orientation | |
| Main aim | Protect overall cognitive function | Target specific cognitive skills | Improve daily functioning | Discuss past events to protect cognitive function | Ensure the patient knows date, time, and their location |
| Delivery method | Group (can also be individual) | Individual | Individual | Individual or group | Individual or group |
| Main benefits | Improves cognitive function in general | Improves targeted cognitive function but is not transferable to other functions | Improves ability to carry out daily tasks | Improves cognitive + emotional symptoms | Improves the patient’s grasp on reality |
| Stages of the disease | Early | Early to moderate | Early to moderate | Early to moderate | Early to moderate |
Another Therapy Option: Cognitive Behavioral Therapy
Cognitive behavioral therapy is not cognitive therapy in the strictest sense. Instead of addressing cognitive issues, cognitive behavioral therapy is a type of talk therapy that aims to help patients understand how their thoughts and feelings can influence their behavior.
This understanding is then used to make positive changes. It has become a popular way of helping dementia patients cope with sleep issues, anxiety, depression, and other mental health problems.
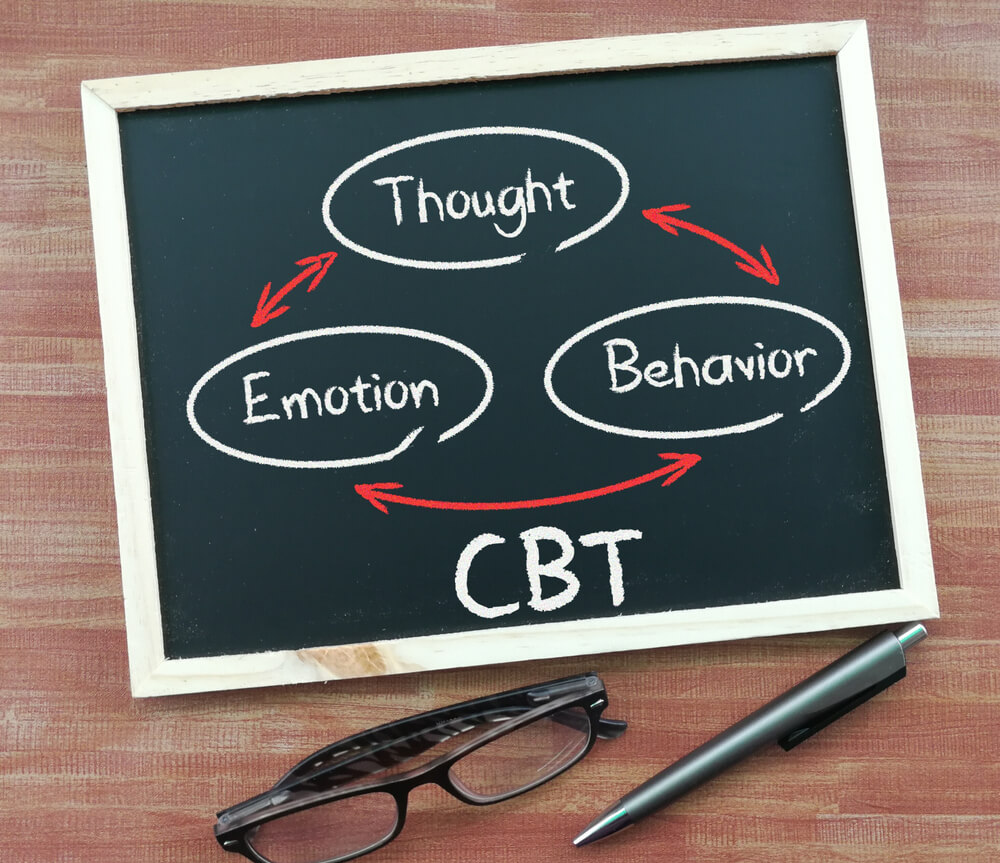
In a typical CBT session, patient and therapist discuss how patients think in certain situations and how that affects the way they feel and act in response. Therapists offer concrete strategies so patients can use the relationship between thoughts, feelings, and actions to iterate to healthier thought patterns and behaviors.
Patients in the early stages of the disease are more likely to respond well to this treatment. Patients with a declining cognitive function may struggle to engage with the therapist due to communication problems, but it’s still possible to adapt CBT to the patient’s level of functioning.
Some of these adaptations include:
- Encouraging patients to repeat information
- Asking questions during the sessions that require the patient to engage their memory. For example, patients may be asked “What is your grandson’s name?” or “What is your phone number?”
- Running shorter sessions of 30–40 minutes, rather than the standard hour
- Only practicing one or two skills per session
- Including the patient’s carer during sessions so that they can repeat exercises at home
- Providing a list of exercises to do at home to practice each skill between sessions
Is CBT Effective for Dementia Patients?
Cognitive behavioral therapy cannot cure dementia, but it can bring symptom relief. For example, brain fog is a common symptom of depression. If CBT is effective against depression, the patient will likely experience reduced brain fog. If the patient uses CBT to combat insomnia and notices improved sleep quality, then any cognitive decline related to poor sleep will likely improve as well.
Most commonly, patients are treated for anxiety and depression, but CBT can also be used for other mental health disorders, including PTSD and insomnia.
Overall, cognitive behavioral therapy can:
- Reduce anxiety, irritability and negative thoughts
- Increase emotional well-being
- Improve communication between patient and caregiver
- Improve quality of life
- Increase engagement in physical and social activities
- Slow down cognitive decline
- Improve quality of sleep and reduce insomnia
Cognitive Activities to Do at Home

Any activities that provide brain stimulation can help patients and slow down symptoms of dementia. For any positive effects to show, these activities need to be carried out consistently and in a structured manner. Activities should be challenging but not impossible to achieve. This helps keep patients motivated and avoids feelings of frustration and failure. Also, patients should be open to engage in as many different activities as possible to help protect different cognitive skills.
Some example activities include:
Engaging in social activities: Socializing with friends and family helps many different cognitive skills, including language and communication skills.
- Go out with friends
- Join a local book or arts and crafts club
- Volunteer at a local charity
- Call friends and family members who live far away
Learning a new skill: Trying something new forces your brain to think and learn new skills. It also requires ongoing follow-up practice to help you improve.
- Learn a new language
- Learn a new sport
- Take up a new hobby
- Learn to play a musical instrument
- Learn a new skill like baking or knitting
- Enroll in an educational or recreational course
Challenging the brain: Engaging in brain-boosting activities can help slow down cognitive decline caused by dementia, including memory, thinking, concentration, verbal fluency, reasoning skills, and others.
- Play strategy board games, like chess
- Solve crosswords, sudoku, anagrams, and word-search games
- Assemble jigsaw puzzles
- Play brain games
- Read books
- Write short stories
Neural Effects uses the latest evidence-based techniques to diagnose and help patients with dementia. We are located in Provo, Utah and serve anyone in the Salt Lake City or Utah County area. We are in network for most types of medical insurance. Schedule your evaluation today.
